The Rocky-Beth Postdoctoral Fellowship Program takes advantage of the unique resources at both Rocky Mountain Laboratories (RML) in Hamilton, Montana, and the main NIH facilities in Bethesda, Maryland, by allowing fellows to have two mentors within NIAID. With more than 2,000 miles separating the two campuses, trainees have the chance to experience two different research environments with complementary research focuses. Meet the Rocky-Beth Fellows who’ve participated since the program was established in 2017.
2021
Johannes Doehl, Ph.D.

Johannes Doehl, Ph.D.
The Laboratory of Malaria and Vector Research Vector Molecular Biology Section and the Laboratory of Bacteriology Tick-Pathogen Transmission Unit, RML
Why did you choose to participate?
The Tick-Pathogen Transmission Unit under Lucas Tirloni, Ph.D., at RML and our group in the Vector Molecular Biology Section under Jesus Valenzuela, Ph.D., at the Twinbrook (near Bethesda) campus have overlapping interests in tick-induced host immunology. As well as the extensive know-how in the area of tick biology and tickborne diseases, RML has unique technical resources that our group can greatly benefit from in our research endeavors. This collaboration was of mutual interest. The Rocky-Beth fellowship offers a unique internal opportunity for fellows to bridge the physical divide between Maryland and RML with the aim of lifting this project off the ground—it was an easy choice to apply for this fellowship.
My research
We are dissecting the host immune response to ticks and Borrelia burgdorferi. The aim is to use cutting-edge technology to determine which part of the immune response is induced by tissue damage, tick-derived molecules, and pathogens like B. burgdorferi. Based on this knowledge, we hope to derive new and targeted interventions against tick-borne pathogen transmission/infection.
Samantha Tilson, Ph.D.
Samantha Tilson, Ph.D.
The Laboratory of Viral Diseases Cellular Biology Section and the Laboratory of Virology Innate Immunity and Pathogenesis Section, RML
Why did you choose to participate?
I truly believe in the collaborative aspect of this program. As an early career scientist, it is extremely important that I establish a niche for myself that I can build my entire career upon. By doing a split postdoc, I am able to capitalize upon the expertise of two different mentors to learn and grow as a scientist without becoming too specialized in any one area. I feel that having three unique perspectives looking at my project is a huge asset. At any given time, at least one of my mentors can act as a fresh set of eyes to look at data in a different way or help focus the project on the salient questions. In addition, working in two different locations allows me to expand my network beyond the main NIH campus and build relationships and learn unique skills that may benefit me later in my career. For example, during my time at RML, I have had the opportunity to work in the biosafety level 3 (BSL-3) laboratory, which is a skill that will benefit me greatly in my future career in virology.
My research
Mitochondria are vital organelles that play key roles in cellular metabolism, innate immune signaling, and apoptotic signaling. Due to the endosymbiotic origins of the mitochondria, damage to these organelles results in the release of danger-associated molecular patterns (DAMPs), which induce inflammation. The goal of my project is to determine how viral manipulation of mitochondrial dynamics contributes to DAMP signaling and inflammation in human tissues using hiPSC-derived liver organoids. Specifically, we are interested in how mitochondrial stress caused by flavivirus infection may be communicated intercellularly and if this stress communication may prime bystander cells for infection. We hope to use hiPSC-derived liver organoids to understand how intercellular stress communication may facilitate viral spread through tissues.
2019/2020
Christine Schneider Lewis, Ph.D.
Christine Schneider Lewis, Ph.D.
The Laboratory of Persistent Viral Diseases Neuroimmunology Unit, RML, and the Laboratory of Malaria and Vector Research Molecular Entomology Unit
Why did you choose to participate?
I have always valued collaborative research that brings together people with diverse scientific backgrounds and interests. I feel like it produces innovative and interesting research directions that answer questions in unique ways. The Rocky-Beth program fits into that niche very nicely and gives me the opportunity to interact with a plethora of researchers in both Montana and Maryland who have very different specialties. In addition, it means I gain exposure to a wider variety of research methods and approaches than I otherwise would, which is invaluable in preparing for the next steps in my career. Although the pandemic has largely reduced my ability to physically travel to Twinbrook to participate in my co-mentor’s lab, I have still benefitted substantially from his advice and mentoring.
My research
The Neuroimmunology Unit at RML studies the neuro-immune factors that cause encephalitis from California Serogroup viruses (CSG viruses). These viruses are carried and transmitted by mosquitoes. Although information has been uncovered about what influences development of severe disease in the brain, we know much less about the initial infection in the skin and have no information about how much the insect vector contributes to disease. The Molecular Entomology Unit studies insect salivary proteins. By forming a collaboration between our labs, we now have the opportunity to explore what impact mosquito salivary proteins have on the skin and brain stages of CSG infection.
Stephen Lu, Ph.D.

Stephen Lu, Ph.D.
Laboratory of Malaria and Vector Research Vector Biology Section and the Laboratory of Bacteriology Plague Section, RML
Why did you choose to participate?
The Rocky-Beth program provides NIH fellows an opportunity to have close contact with two distinct research groups, bridging their knowledge and experiences toward a shared scientific question. Having two mentors enhances the quality of the candidate’s postdoctoral experience. From the technical perspective, the candidate has access to and can be trained in a broader set of skills by taking advantage of the expertise within each group. Additionally, frequent discussions with each mentor improve the candidate's ability to have a “big picture” view over the topic of study and also aid the candidate to approach the project from more than one perspective. Finally, having two mentors can be very instructive in other relevant topics by offering different examples of leadership and on how to conduct and deal with day-to-day laboratory issues, which are important aspects of the scientific career.
The program also offers an additional funding opportunity for the group, allowing more flexibility and responsibility to the candidate's project. In addition, to participate in the Rocky-Beth program, the candidate must write a grant proposal, inviting the candidate to practice and improve their grant writing abilities.
Long story short, the Rocky-Beth program offers the possibility for a solid and distinct postdoctoral training.
My research
The rat flea Xenopsylla cheopis is the main vector of Yersinia pestis, the etiological agent of the bubonic plague. In addition to Y. pestis, fleas can also transmit other medically relevant pathogens including Rickettsia spp. and Bartonella spp. However, despite the historical and clinical importance of X. cheopis, little is known regarding their salivary gland contents and potential activities. Therefore, the objective of our project is to investigate X. cheopis salivary gland content by transcriptomic and proteomic approaches, in addition to characterizing molecules with potential pharmacological activities.
2018
Rebecca Broeckel, Ph.D.
Rebecca Broeckel, Ph.D.
The Laboratory of Virology Innate Immunity and Pathogenesis Section, RML, and the Laboratory of Molecular Microbiology Nonhuman Primate Virology Section
Why did you choose to participate?
After my Ph.D., I wanted to focus on innate immunity to emerging viruses, and a partnership with Sonja Best, Ph.D., in the Laboratory of Virology at RML was a great fit—I have also had the unique opportunity to work in a biosafety level 4 (BSL-4) facility.
My research
I study how mosquito antiviral immunity impacts arbovirus transmission. I am studying how Aedes aegypti Piwi proteins interact with viral small RNA populations. We are interested in how these interactions impact long-term antiviral immunity and what they reveal about Piwi protein evolution and functional divergence across organisms.
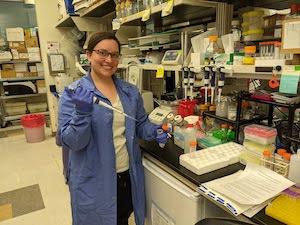
Shayla Hesse, M.D.
Laboratory of Bacteriology, Pathogen-Host Cell Biology Section, RML and the Laboratory of Molecular Biology at the National Cancer Institute
2017
Rahul Basu, Ph.D.

Rahul Basu, Ph.D.
The Laboratory of Immune System Biology Signaling Systems Section and the Laboratory of Persistent Viral Diseases Neuroimmunology Unit, RML
Why did you choose to participate?
Rocky-Beth Fellowship program is one of the most innovative ways of creating collaboration between RML in Montana and the NIH main campus in Bethesda. I first learned about this program through Karin Peterson, Ph.D., my current PI in RML. Following this encounter, Iain Fraser, Ph.D., Dr. Peterson, and I started working on conceptualizing a project that involved two NIAID laboratories—the Rocky-Beth Fellowship was the perfect opportunity for this project. I started working in RML to establish a model of neurotropic virus infection as well as the opportunity to travel to the main campus to understand what could be done to pursue further mechanistic investigations. We shared ideas and plans during the visits and online meetings. Based on this, we established a viral model in RML and started dissecting the mechanisms involved in viral entry into the brain. Followed by that, I moved to the main campus for targeted follow-up studies with the aim to design putative therapeutic strategies. Both laboratories are unique in regard to the type of work that is conceptualized and performed and the technologies used regularly. Thus, the Rocky-Beth Fellowship provided an immense opportunity to learn and be trained by both of laboratories situated in very different parts of the United States. In my opinion, the collaborative project we carried out utilizing the Rocky-Beth Fellowship is scientifically significant and impactful.
My research
We worked on La Crosse virus (LACV), which causes pediatric arboviral encephalitis by selective disruption of blood-brain barrier in children. We see a similar phenotype in mice where the weanling mice are susceptible, but the adult mice are not. In our project, we tried to understand what’s causing the selective blood-brain barrier leakage in weanling mice but not in adults. In RML, we established a model of LACV infection and related leakage using the brain capillary endothelial cells (Basu et al., J Neuroinflammation, 2021). Utilizing this model, we have done transcriptome-wide and targeted screening to understand the genes/proteins and pathways involved in this. Finally, these molecules are giving us a lead to potential therapeutic strategies that can be implemented in LACV-induced encephalitis.
Emily Speranza, Ph.D.

Emily Speranza, Ph.D.
The Laboratory of Virology Innate Immunity and Pathogenesis Section, RML, and the Laboratory of Immune System Biology Lymphocyte Biology Section
Why did you choose to participate?
As I was nearing the end of my Ph.D. I had the good fortune to meet with Sonja Best, Ph.D. The work done in her lab had always interested me, and so did the possibility of doing a postdoc with her group. While discussing how our works could move forward in combination, we concluded that our analyses of tissue immunity by transcriptional response would be greatly complemented by analysis of cell spatial organization during infection. This is how the Rocky-Beth Fellowship Program entered the conversation, and the collaboration with Ronald N. Germain, M.D., Ph.D., whose lab specializes in tissue immunity through looking at the organization of the cells.
The chance to learn from both mentors for a unique postdoc experience made the decision to join the Rocky-Beth Program an easy one. It was especially enticing because it would give me the opportunity to expand my knowledge of transcriptional response in addition to learning and applying a skill that I found to be interesting and an important component of a well-rounded analysis of the host response to infection. I would gain experimental knowledge in the two major fields I wanted to study, virology and immunology, while providing ample opportunity to continue to expand my computational skills. In addition, by the mixture of influences from two separate fields and labs, I was able to create a research program that is easily distinguishable from the work of either mentor involved, aiding me in achieving independence for a future career. This was made possible by the Rocky-Beth Fellowship Program.
My research
The major goals of my research as an independent research scholar are to investigate the tissue-level immune responses to emerging RNA virus infections. The work is focused on trying to understand the spatial-temporal and transcriptional responses to very early virus infections all with a single-cell resolution. To achieve this, I combine high-content tissue imaging of whole tissue sections with single-cell RNA sequencing technologies to understand the major questions of which cells are getting infected in the tissue, which cells are responding to the infection, and how the spatial organization of the tissue changes over time. This has been applied to the study of Ebola virus, vesicular stomatitis virus, and SARS-CoV-2. Radtke AJ, Kandov E, Lowekamp B, et al, Proc Natl Acad Sci U S A., 2020 and Speranza E, Williamson BN, Feldmann F, et al., Sci Transl Med. 2021

