NIAID’s VRC, S. Africa’s Afrigen Kick Off Vaccine-Sharing Efforts
Training Aimed at Making mRNA Technology Available Globally
A team of vaccine production experts from South Africa recently finished training in Maryland as part of a global mRNA vaccine collaboration. The experts are working with scientists at NIAID’s Vaccine Research Center (VRC) to produce vaccines against a list of troubling infectious diseases.
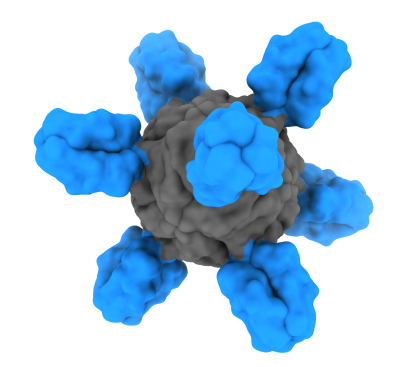
The mRNA vaccine platform, which became commonly used during the COVID-19 pandemic, works by delivering a piece of genetic material to cells that instructs the body to make a protein fragment resembling one from a target pathogen (such as a virus). The immune system then recognizes and remembers the fragment, enabling it to mount a strong response if the body is exposed to that pathogen. The mRNA vaccine production process involves inserting the selected virus protein gene into a plasmid (a circular piece of DNA), the production of which was the topic of the visit from the South African scientists.
The seven-member team from Afrigen Biologics and Vaccines, a biotechnology company based in Cape Town, South Africa, arrived on July 21 for two weeks of collaboration and learning with VRC scientists. They focused on vaccine manufacturing at the VRC’s Vaccine Clinical Materials Program in Frederick, Maryland. Specific aspects included topics such as: inoculum growth, nutrient feeding, quality control, and other steps needed to make an mRNA vaccine. The Afrigen team also met with VRC leadership, including the recently appointed VRC Director, Dr. Ted Pierson.
The visit represented a significant milestone for an ongoing research collaboration established in March 2022 between NIAID and Afrigen. Their objective is to share knowledge, expertise, and data to expedite mRNA vaccine production globally. As part of the collaboration, NIAID – specifically scientists at the VRC – are making plasmid DNA that will be used for Afrigen’s in vitro transcription process. Additionally, the VRC is providing technology transfer and training on plasmid DNA manufacturing, which the Afrigen group observed during the visit. In turn, Afrigen is sharing knowledge and expertise with NIAID scientists about the in vitro transcription and lipid nanoparticle formulation processes. The mutually beneficial scientific collaboration will advance each institution’s work toward establishing mRNA vaccine production capabilities to support their respective missions.
The World Health Organization, the COVAX Vaccine Manufacturing Taskforce, and the Medicines Patent Pool established a formal agreement in July 2021 to build capacity in low- and middle-income countries to make mRNA vaccines, now known as the mRNA technology transfer programme. Afrigen was chosen as a center of excellence and training, or “technology transfer hub,” as part of the mRNA technology transfer programme. The hub is designed to improve the health and security of member nations by creating sustainable, locally owned mRNA vaccine manufacturing in those nations. Because mRNA vaccines can be cheaper to produce, quickly developed in response to outbreaks, and easily modified when new variants of pathogens emerge, the ability to produce these vaccines in low- and middle-income nations will contribute significantly to global health security.
Afrigen is working to establish mRNA vaccine production technology—initially for a COVID-19 vaccine candidate—and will work with local partners to conduct research to evaluate the vaccines, along with manufacturing the vaccines at scale. The eventual goal is to be able to share this established process with manufacturers across multiple countries.
Though the effort began with COVID-19 in mind, the scientists are mutually hoping to use the mRNA vaccine platform to develop and test vaccines against an array of infectious diseases found globally, such as HIV, tuberculosis, malaria, influenza, cancer-associated viruses and more.

Afrigen scientists spent time getting to know colleagues at the Vaccine Research Center’s Vaccine Production Program (VPP) and Vaccine Clinical Materials Program (VCMP), including during a meet-and-greet with VRC leadership and staff at the VCMP pilot plant in Frederick, Maryland.