An HIV vaccine candidate elicited trace levels of HIV broadly neutralizing antibodies (bNAbs) and high levels of other key immune cells in an early-stage clinical trial. This immune response is an important signal that, if antibody levels can be further amplified, the vaccination strategy might be able to prevent HIV. The findings of this NIAID-supported trial were published in the journal Cell.
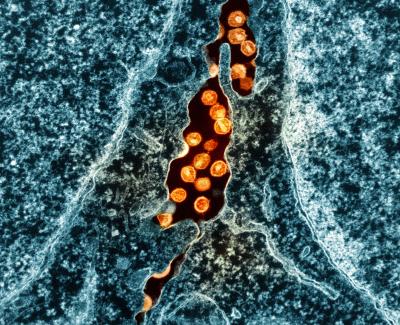
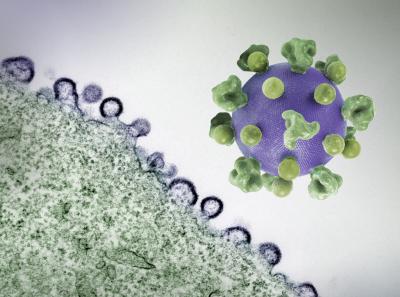
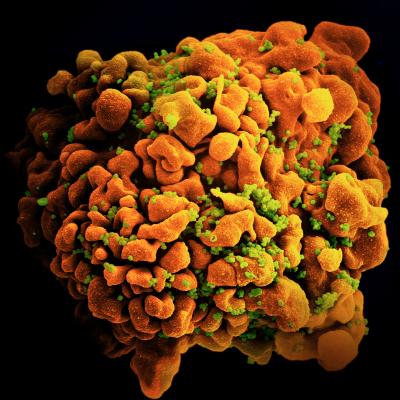
HIV has genetic diversity that makes it difficult to target with a vaccine, but bNAbs are thought to be key to overcoming that hurdle because they bind to parts of the virus that remain relatively stable even when it mutates. Several classes of HIV-specific bNAbs have been identified, and each class binds to a different stable section of the virus’ surface. Some people with HIV generate bNAbs naturally through a process that typically occurs over years. For a preventive vaccine, researchers seek to accelerate the process by which the immune system generates bNAbs and to do so in people who do not have HIV.
The clinical trial examined the ability of a vaccine concept to elicit bNAbs that bind to the membrane proximal external region (MPER) of an HIV surface protein. The study enrolled 24 participants, of whom 20 were randomly selected to receive vaccine doses. The remaining four participants received placebo injections. Fifteen participants in the vaccine arm received two doses, and five participants received three doses. The team then analyzed study participant blood samples.
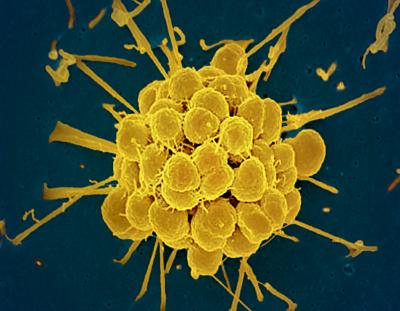
They found that 13 vaccine recipients generated early-stage MPER-directed antibodies after two doses. Among the five participants who received three doses, the antibodies in samples from two of them could neutralize many common globally circulating HIV strains in vitro, i.e., in a test tube or culture dish. One of those two participants had B cells—immune cells that produce antibodies—showing signs of maturing in such a way that they would be able to produce MPER-directed bNAbs if stimulated further. The other participant had started producing MPER-directed bNAbs. Vaccine recipients also had evidence of CD4+ T cell activity, which is a crucial step in enabling antibody development. One vaccine recipient experienced anaphylaxis, a known but rare allergy-related adverse event, which was promptly managed and resolved. The team investigated the cause of the event, which was likely from an additive used to help stabilize the vaccine contents. The trial was halted at that time.
The research was sponsored by NIAID, co-funded by the Bill & Melinda Gates Foundation, and conducted by the Duke Consortium for HIV/AIDS Vaccine Development (CHAVD), one of two NIAID-supported HIV vaccine consortia, in collaboration with the NIAID-funded HIV Vaccine Trials Network. This study provided the proof of concept that a vaccine can induce bNAbs in people, which is a key question being pursued in the HIV vaccine research field. Moreover, bNAbs were detected within weeks, which is much faster than the antibody response in people with HIV. According to the authors, it is likely that an effective vaccine will need to build on and amplify the immune response that was observed in this study. Together, the clinical trial results identified ways that the vaccine’s safety and efficacy must be enhanced before it advances through further evaluation, and a new vaccine candidate is being developed based on these findings.
NIAID is grateful to the research teams and volunteers who participate in HIV vaccine studies.
For more information about this study, please visit ClinicalTrials.gov and use the study identifier NCT03934541.
Reference
W Williams et al. Vaccine induction of heterologous HIV-1-neutralizing antibody B cell lineages in humans. Cell DOI: 10.1016/j.cell.2024.04.033 (2024)