An HIV drug that suppresses the activity of the CCR5 receptor—a collection of proteins on the surface of certain immune cells—was associated with better renal function in kidney transplant recipients with HIV compared to people who took a placebo in a randomized trial. Study participants taking the drug, called maraviroc, also experienced lower rates of transplant rejection than those taking placebo, but the difference was not statistically significant due to lower-than-expected rejection rates across the entire study population. The findings of the NIAID-sponsored trial were presented today at the 2024 American Transplant Congress in Philadelphia.
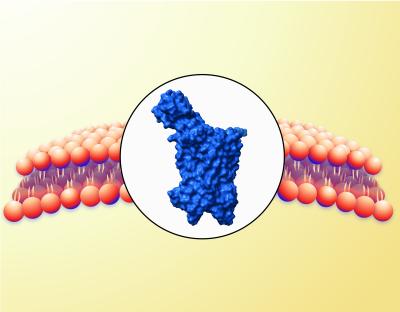
The CCR5 receptor helps HIV enter CD4+ T cells. Some people have a genetic mutation that prevents the CCR5 receptor from working, and either cannot acquire HIV or experience slower HIV-related disease progression if living with the virus. It has separately been observed that people with the same CCR5 genetic mutation have better outcomes following kidney and liver transplantation. The CCR5 antagonist class of antiretroviral drugs was developed to mimic the naturally occurring CCR5 mutation and is a well tolerated component of HIV treatment, but the drugs have not been evaluated as an intervention to improve transplantation outcomes in people. Furthermore, transplant recipients with HIV more frequently experience transplant rejection and elevated CCR5 activity than transplant recipients without HIV.
A research team led by the University of California San Francisco conducted a U.S.-based Phase 2 trial to assess the safety and tolerability of the CCR5 antagonist maraviroc given daily from the time of transplant onward among kidney transplant recipients, and to compare renal function of people taking daily maraviroc to those taking a placebo one year (52 weeks) post-transplant. All study participants were living with HIV and were virally suppressed on antiretroviral therapy (ART) regimens. The study randomized 97 participants to receive maraviroc or a placebo in addition to their continued ART regimens post-transplant. Of them, only 27 participants were able to complete all necessary study examinations through 52 weeks due to logistical complications from the SARS-CoV-2 pandemic. At one-year post-transplant, the mean estimated glomerular filtration rate—a measure of how well kidneys were working—was significantly higher in participants receiving maraviroc in addition to their ART regimen compared with participants receiving ART and placebo (59.2 versus 49.3 mL/min/1.73m2). The drug was safe and well tolerated.
Four of the 49 participants taking maraviroc and 6 of the 48 participants taking placebo experienced transplant rejection, but this difference was not statistically significant given the relatively small sample size. Transplant rejection rates were lower than expected across both study groups, which the study team suggests may be a favorable outcome of the ART regimens most participants were taking.
The addition of maraviroc significantly improved renal function in kidney transplant recipients with HIV compared to placebo. According to the authors, these findings warrant further exploration of the benefit of CCR5 antagonists in all kidney transplant recipients regardless of HIV status.
For more information about this study, please visit ClinicalTrials.gov and use the identifier NCT02741323.
Reference:
Brown et al. Beneficial Impact of CCR5 Blockade in Kidney Transplant Recipients with HIV. American Transplant Congress in Philadelphia, Pennsylvania. Tuesday, June 4, 2024.