Tolerance is the prevention of an immune response against a particular antigen. For instance, the immune system is generally tolerant of self-antigens, so it does not usually attack the body's own cells, tissues, and organs. However, when tolerance is lost, disorders like autoimmune disease or food allergy may occur. Tolerance is maintained in a number of ways:
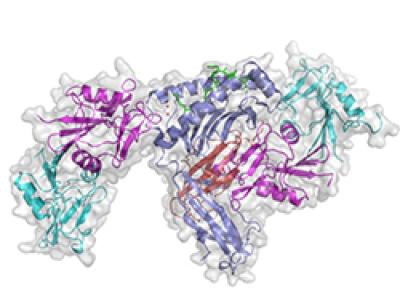
Inhibitory NK cell receptor (purple and light blue) binds to MHC-I (blue and red), an interaction that prevents immune responses against self.
- When adaptive immune cells mature, there are several checkpoints in place to eliminate autoreactive cells. If a B cell produces antibodies that strongly recognize host cells, or if a T cell strongly recognizes self-antigen, they are deleted.
- Nevertheless, there are autoreactive immune cells present in healthy individuals. Autoreactive immune cells are kept in a non-reactive, or anergic, state. Even though they recognize the body's own cells, they do not have the ability to react and cannot cause host damage.
- Regulatory immune cells circulate throughout the body to maintain tolerance. Besides limiting autoreactive cells, regulatory cells are important for turning an immune response off after the problem is resolved. They can act as drains, depleting areas of essential nutrients that surrounding immune cells need for activation or survival.
- Some locations in the body are called immunologically privileged sites. These areas, like the eye and brain, do not typically elicit strong immune responses. Part of this is because of physical barriers, like the blood-brain barrier, that limit the degree to which immune cells may enter. These areas also may express higher levels of suppressive cytokines to prevent a robust immune response.
Fetomaternal tolerance
Fetomaternal tolerance is the prevention of a maternal immune response against a developing fetus. Major histocompatibility complex (MHC) proteins help the immune system distinguish between host and foreign cells. MHC also is called human leukocyte antigen (HLA). By expressing paternal MHC or HLA proteins and paternal antigens, a fetus can potentially trigger the mother's immune system. However, there are several barriers that may prevent this from occurring: The placenta reduces the exposure of the fetus to maternal immune cells, the proteins expressed on the outer layer of the placenta may limit immune recognition, and regulatory cells and suppressive signals may play a role.
Read more about MHC proteins in Communication.
Transplantation
Transplantation of a donor tissue or organ requires appropriate MHC or HLA matching to limit the risk of rejection. Because MHC or HLA matching is rarely complete, transplant recipients must continuously take immunosuppressive drugs, which can cause complications like higher susceptibility to infection and some cancers. Researchers are developing more targeted ways to induce tolerance to transplanted tissues and organs while leaving protective immune responses intact.

