NIAID-supported research has contributed to great increases in the number and efficacy of autoimmune disease treatment approaches available. Even so, unmet needs remain. These include:
- Immune therapies that are less toxic and create less risk of infection.
- Precision approaches for selecting the right therapy for each person with autoimmune disease.
- Treatment options for people who don’t respond to current therapies.
- Treatments that delay or prevent the onset of disease.
Reducing the Risk of Infection and Other Toxicities
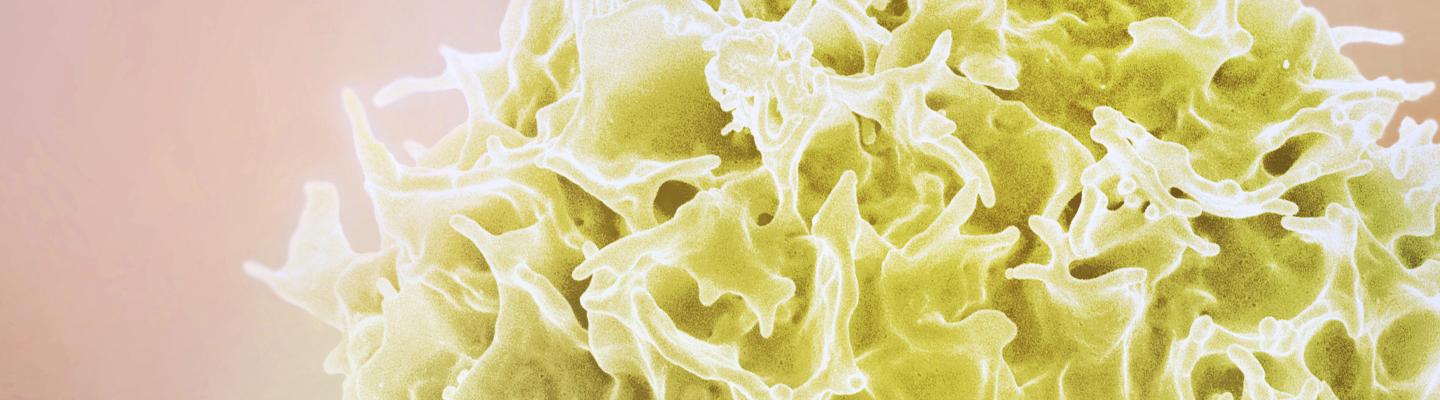
Many currently available therapies for autoimmune disease suppress the immune system. As a result, these medications can treat the disease but have the side effect of making people more vulnerable to infections. NIAID-supported research on autoimmune disease treatment aims to suppress autoimmunity in a targeted way so the immune system can continue to fight viruses and other pathogens effectively. One experimental strategy is to eliminate only those cells that attack healthy tissue, called autoreactive cells, while retaining cells that protect tissue from infection and cancer. Another strategy under research uses vaccines to convert autoreactive cells into cells that protect the target tissue instead. This strategy also has the potential to cure people of autoimmunity.
In addition, researchers are exploring whether people can successfully manage their autoimmune disease symptoms while reducing or tapering off their immunosuppressive medication. Doing so would reduce their susceptibility to infection and to side effects from long-term use of medication. Learn about a study of this approach to the treatment of systemic lupus erythematosus in the NIAID News.
The Right Therapy for Each Person
The wide variation in biological mechanisms that cause autoimmune diseases, even among people with the same disease, makes it challenging for healthcare providers to predict which therapy will work best for each person. To help overcome this problem, NIAID supports research designed to use scientists’ understanding of these mechanisms to help healthcare providers diagnose a person’s autoimmune disease and choose the appropriate therapy. This research includes identifying easily detectable biological clues that reveal the mechanisms underlying a person’s disease.
Unfortunately, some people do not respond to currently available therapies. NIAID's focus on supporting research to understand the immune processes behind autoimmunity is anticipated to lead to the identification of novel therapeutic options for these people.
For severe cases of autoimmune disease, NIAID supports clinical trials of a blood stem cell treatment. This treatment involves removing immune cells that attack the body and repopulating the immune system, allowing it to reset itself so the new immune cells no longer attack healthy tissue. Learn about the current trial of this approach to treating severe forms of relapsing multiple sclerosis.
Delaying or Preventing the Onset of Disease
A long-term goal of NIAID is to stop autoimmunity even before disease becomes apparent. To achieve this goal, NIAID funds research on the immune processes underlying the very early stages of autoimmunity. These studies may enable discovery of biological markers and treatment targets that lead to the development of diagnostics and therapies that help delay or prevent the onset of autoimmune diseases.
Delaying the Onset of Type 1 Diabetes
Since the discovery in the 1970s that the immune system causes type 1 diabetes (T1D), NIAID and other NIH institutes have funded studies aimed at developing medications to treat and prevent the disease. Some of this research culminated in the 2022 approval by the Food and Drug Administration of the first medication to delay the onset of T1D. Additional research is needed to identify agents that could further delay and ideally prevent the disease.
T1D occurs when the immune system’s T cells attack insulin-producing beta cells in the pancreas. These T cells have a protein on their surface called the CD3 receptor. NIAID-funded researchers discovered in 1979 that an antibody called OKT3 binds to the CD3 receptor, slowing the attack on beta cells. A decade later, scientists supported by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and others learned that treating mouse models of diabetes with an anti-CD3 antibody delayed disease onset, but OKT3 caused negative side effects in humans. Researchers discovered how OKT3 caused these side effects and designed a safer antibody in studies funded by NIAID and NIH’s National Cancer Institute in the 1990s. Subsequently, clinical trials funded by NIAID, NIDDK, and others evaluated this antibody, called teplizumab, eventually testing its efficacy in children with T1D. These trials led to FDA approval of teplizumab in 2022 as the first drug to delay T1D onset. View an infographic illustrating this research journey on the NIAID website.
While the approval of teplizumab was a major advance, the medication does not work for everyone who receives it. Research is needed to find biological markers that help doctors identify which people at risk for T1D will respond to teplizumab. In addition, the treatment delays the onset of T1D for two to three years at most. Scientists hope to identify medications that can be paired with teplizumab to make it more effective for more people.