The NIAID Pandemic Preparedness Plan builds on a foundation of pathogen-specific research that include advancing research on priority pathogens known to or having the potential for emerging as public health threats. Continuing to build a robust basic research portfolio and advancing translational science on these pathogens is essential for biomedical preparedness. In addition to known threats, effective preparedness must also account for unexpected emerging disease threats, commonly referred to as Pathogen(s) X. To mitigate risks associated with these yet unknown pathogens, NIAID will prioritize preparedness research on prototype-pathogens, which are select pathogens identified from viral families known to infect humans. Viruses are taxonomically organized into families based upon shared functional and structural similarities. Because of this, candidate vaccines developed against a prototype pathogen from a family may similarly work against other members in the same family. Through targeted basic and applied research on these prototype pathogens from each viral family of concern, the accrual of a solid foundation of knowledge and medical countermeasures (MCMs), such as therapeutics, vaccines, and monoclonal antibodies (mAbs), will enable a rapid response when a Pathogen X emerges from any of the viral families of concern. This anticipatory approach will exponentially increase the preparedness and response portfolio and enable rapid movement of candidate MCMs into clinical trials.
NIAID will support the research, development, and testing of critical MCMs through Phase I/IIa clinical trials where appropriate, in coordination with other entities undertaking similar research worldwide. NIAID also will continue to provide the USG public health infrastructure with a robust pipeline of preparedness resources to shorten the response timeline when human viral disease threats emerge. NIAID, the lead NIH Institute for infectious disease research and MCM discovery, has broad capacity in infectious diseases and immunology and a history of preparing for and responding to domestic and global infectious disease threats. A central NIAID team will facilitate, coordinate, and harmonize preparedness research and development within the Institute. It also will communicate and coordinate with the NIH and other relevant USG agencies as well as appropriate entities outside the U.S., including key international organizations and foreign research partners.
To prevent widespread morbidity and mortality, the early detection of an emerging pathogen threat is essential. Therefore, in partnership with the CDC, USAID and other USG entities concerned with emerging infectious diseases, strategic epidemiological field studies undertaken by NIAID-supported centers and networks will provide key reagents and insights into viruses that have the potential to cause a human epidemic or pandemic. In addition, these efforts will be coordinated with similar global efforts already underway or planned so that informed worldwide surveillance and epidemiology is assured.
Technological advancements, such as platform technologies for MCMs, will also be crucial to the preparedness effort. The most promising platform technologies will need to be leveraged for development of vaccines, therapeutics, and diagnostics. Their products will also need to be evaluated clinically through an experienced and nimble clinical trial infrastructure that complies with rigorous regulatory standards. Developing and leveraging these cross-cutting elements across the preparedness research pipeline will enable NIAID to support the USG research effort that will underpin an effective response to public health emergencies caused by emerging or re-emerging infectious disease threats.
Preparedness-Response Continuum
Pandemic preparedness and response exist along a continuum, and it is important to operationally distinguish between the capacities associated with each. The extent of preparedness will determine the speed and effectiveness of a response. The NIAID preparedness research efforts will provide the reagents, roadmaps for product development and evaluation, scientific infrastructure, and study capacity needed for a robust research response to a future pandemic.
Conceptual Approach
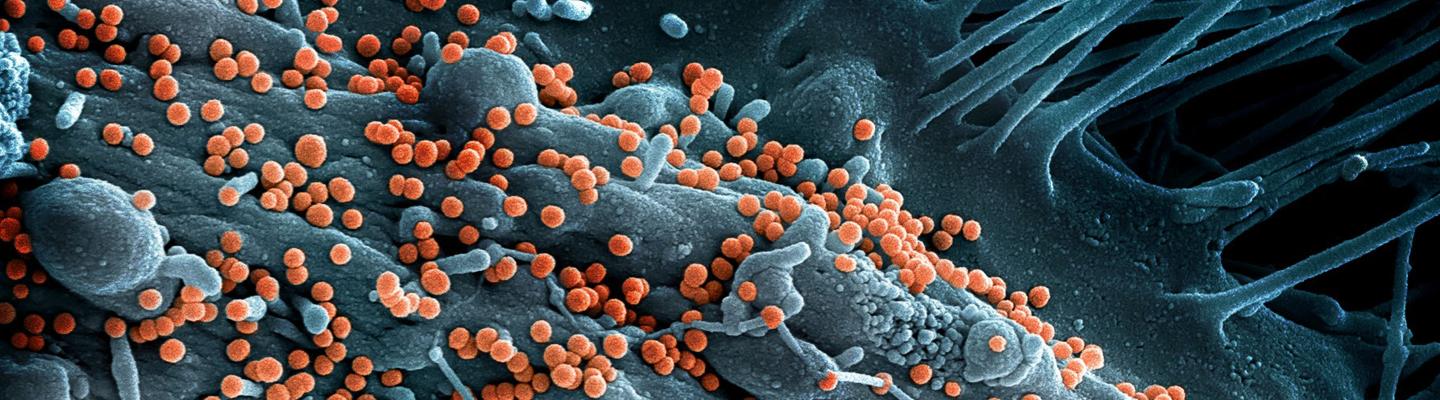
Preparedness for major infectious disease outbreaks will save lives; rapid deployment of effective diagnostics, vaccines, and treatments can contain an outbreak before it expands into a larger epidemic or pandemic. Obtaining in-depth knowledge and developing MCMs for prototype pathogens within viral families that pose the highest risk for epidemics/pandemics is an effective strategy to prepare for future disease outbreaks. This approach was successfully applied during the global COVID-19 pandemic of 2020 when prior knowledge gained through the study of SARS-CoV-1 and MERS-CoV was leveraged to rapidly design vaccines, diagnostics, and therapeutics against SARS-CoV-2.
Priority and Prototype Pathogen Research
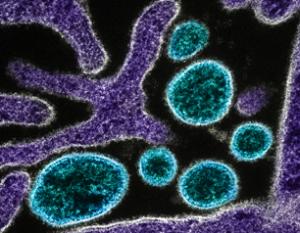
There are multiple virus families for which there are no available licensed vaccines, and many member viruses within families that have potential to cause significant human disease. Since it is not feasible to fully characterize the ~120 viruses known to cause human disease and develop MCMs for each, selection of representative viruses from each family offers a viable pathway to gain knowledge that may be applicable to part or all of a particular virus family. These representative viruses are considered prototype pathogens. For example, within the Arenaviridae family, Lassa, Junin, or other viruses could be selected as a prototypic pathogen(s). The ideal arenavirus prototype pathogen(s) would not only be a virus with a risk of causing an outbreak, but most importantly, would be one that shares functional and structural properties with viruses across the Arenaviridae family. Thus, increasing fundamental knowledge and developing MCMs for the prototype virus(es) not only provides ready potential solutions for these viruses, but also the framework for a rapid research and product development response to other viruses within that family should an outbreak occur. A schematic for how prototype pathogens are selected, studied, and brought to clinical trials is shown in Figure 1.
In addition to the prototype pathogen approach, NIAID will also characterize, develop reagents, and conduct pre-clinical and clinical testing of other pathogens that may not serve as prototypes, but that nonetheless threaten human health and thus are considered a high priority to study. We refer to these as priority pathogens. This pathogen-specific research prioritizes viruses most likely to cause significant human morbidity and mortality. While priority pathogens can also be prototype pathogens (e.g., Ebola virus), these two designations do not necessarily overlap. For instance, Zika virus of the Flaviviridae family is known to cause human morbidity, but it does not serve as a good prototype for development of MCMs for other Flaviviridae family members. Thus, NIAID will continue to support Zika virus research in the capacity of a priority pathogen. To ensure adequate coverage of viruses that pose a known threat to human health and Pathogen(s) X, NIAID will support both priority and prototype pathogen research through its pandemic preparedness strategy.
Research and Development
The Pandemic Preparedness Plan will support critical studies to characterize prototype and priority pathogens, including understanding viral biology and structure, host immune responses, mechanisms of immune evasion, disease pathogenesis, and studies to develop assays and animal models of disease. Research and development will encompass preclinical and translational activities and will include expanded conduct of early phase clinical studies to evaluate candidate countermeasure safety and immunogenicity, or drug profile characteristics. Clinical trials of promising MCMs will include equitable representation of participants from traditionally underrepresented groups, all sexes, and individuals across the lifespan.