Add Staphylococcus epidermidis to the list of common human bacteria undergoing an image change: From bad reputation of “disease causing” to something helpful – and likely interesting to probiotic users.
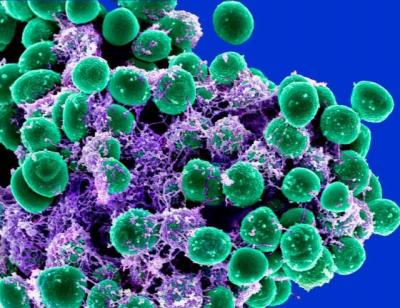
S. epidermidis is known as a bacterium that usually colonizes harmlessly on the skin, but can be dangerous when it invades deeper, say through a cut or – more commonly – a surgical implant, such as a catheter. Once established internally, the bacterium can form biofilms that are difficult to treat with antibiotics. S. epidermidis is of particular concern in healthcare settings because it often spreads easily in people who are ill or have weakened immune systems.
The bacterium’s new image is aided by research findings just published by NIAID scientists and colleagues in Cell Host and Microbe. The group showed that S. epidermidis produces enzymes, known as sphingomyelinase, that help the bacteria acquire nutrients and colonize the skin. But the bacterial enzymes also help the skin produce ceramides, which are important components of the outer skin layers that prevent drying and aging of the skin. Low ceramide levels contribute to many skin diseases, such as atopic dermatitis, commonly called eczema. With colleagues from Shanghai Jiaotong University in China, the NIAID scientists identified how the mutually beneficial relationship works.
The study used research mice and samples from the faces and armpits of human volunteers to verify that S. epidermidis produces sphingomyelinase and that the enzyme is not harmful. In the mice, they then found that the presence of S. epidermidis on the skin significantly increases ceramide levels and prevents water loss from damaged skin. Then they discovered that these processes are entirely dependent on the sphingomyelinase that the bacteria secrete.
Their study points out that – much like in the gut, where scientists are learning about the balance between good and bad bacteria – the same type of harmony takes place on the skin.
“Our study underlines the potential translational use of S. epidermidis in a probiotic fashion to promote skin health during aging or in people suffering from skin diseases such as atopic dermatitis,” the authors state. Such an undertaking would involve a complex clinical trial involving hospitals and clinicians, so nothing is set, though the scientists plan to discuss how and where such a study could proceed. Another NIAID research team has shown in a small study that a probiotic therapy reduced severity of eczema symptoms in children.
Reference: Y Zheng, et al. Commensal Staphylococcus epidermidis contributes to skin barrier homeostasis by generating protective ceramides. Cell Host and Microbe (2022).