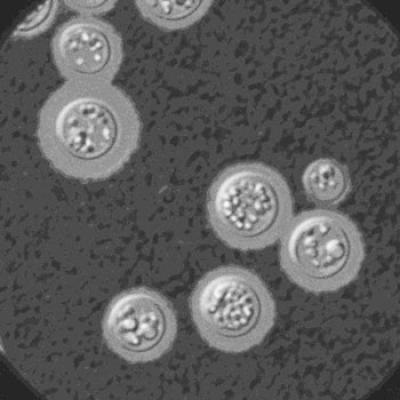
The fungus Cryptococcus neoformans can cause brain inflammation, or meningitis.
In a new study, NIAID researchers describe the immune responses of healthy people who developed the fungal infection cryptococcosis. The researchers found that disease progression in otherwise healthy people differs from those who develop the infection due to complications that compromise the body’s immune system, like HIV infection. Therefore, different therapies should be explored for people without underlying infections. The study appears in the May 28, 2015, edition of PLOS Pathogens.
Burden and Benefit
The fungus Cryptococcus, a type of yeast, is responsible for cryptococcal meningitis, a potentially fatal fungal brain infection. The majority of cases and fatalities occur in immune-compromised people, including those with HIV and patients taking immunosuppressive drugs. However, in the United States approximately one-third of cases fall outside these groups, and relatively healthy people are infected for unknown reasons. Up to 30 percent of non-HIV cases in the United States are fatal, despite treatment. Understanding the cause and progression of cryptococcosis in non-HIV cases will enable researchers to offer more effective treatments for this debilitating disease.
Background
Cryptococcosis most often presents as an opportunistic infection in people infected with HIV, who are more susceptible to the fungal infection because HIV disrupts essential infection-fighting immune cells called T cells. Others with suppressed immune systems, such as organ transplant recipients on immunosuppressive drugs, also are susceptible to the disease. People with cryptococcosis may develop meningitis, which can lead to loss of consciousness and severe weakness, or “locked-in syndrome,” a state of paralysis.
A Puzzling Success
Peter Williamson, M.D., Ph.D., chief of the Translational Mycology Unit in the Laboratory of Clinical Infectious Diseases, led NIAID researchers in seeking to uncover why healthy people may be susceptible to Cryptococcus and why therapies so frequently fail these patients. Immune-activating therapies currently are recommended for combatting severe cases of cryptococcosis, because many people with the fungal infection have compromised immune systems. However, the NIAID researchers observed that steroids, which suppress components of the immune system, led to positive outcomes for two otherwise healthy people who developed cryptococcosis and were undergoing active therapy for their infection. These paradoxical observations provided the basis for exploring the immune response in non-HIV cases.
Results of Study
The team collected samples, including spinal fluid and blood, from cryptococcosis patients at the National Institutes of Health Clinical Center who did not have HIV or other underlying conditions. In contrast to what is observed in HIV cases, non-HIV spinal fluid samples had expansion of T cells and many other types of immune cells. Markers of inflammation produced by these cells were elevated, as was NFL, a biomarker of neuron damage. Although antifungal therapies kill Cryptococcus, small pieces of the fungus remain and can provoke immune responses. The scientists’ findings suggest that an overly active inflammatory response to the fungus during therapy results in brain swelling and neuronal damage, which could be subdued with immune-suppressing steroids.
In addition, the NIAID team analyzed brain biopsies and found that immune cells called macrophages, which normally respond to signals from T cells to engulf and kill fungi, instead responded as if to an allergic reaction. This defective macrophage response failed to clear the fungal infection.
Putting these two pieces of information together, the researchers proposed that defective macrophages in otherwise healthy people result in susceptibility to cryptococcal infection. Fungal components released during treatment result in an excessive T-cell response in these patients, which leads to brain swelling and damage.
Overall, the study shows that non-HIV immune responses to cryptococcosis differ greatly from those of HIV patients and should be explored in detail. More research will clarify how best to control the overly aggressive T-cell immune response and identify factors underlying the macrophage defects that may have led to the original susceptibility to the infection.
Next Steps Toward Discovery
The researchers will be developing new methods to evaluate and treat people with non-HIV cryptococcosis in an ongoing clinical trial, which has a broader goal of understanding why healthy people develop cryptococcosis. The trial also includes the relatives of people with cryptococcosis to help determine potential genetic factors that may cause susceptibility to the fungus.
Reference
Panackal AA, Wuest SC, Lin YC, Wu T, Zhang N, Kosa P, Komori M, Blake A, Browne SK, Rosen LB, Hagen F, Meis J, Levitz SM, Quezado M, Hammoud D, Bennett JE, Bielekova B, and Williamson PR. Paradoxical immune responses in non-HIV cryptococcal meningitis. PLOS Pathogens (2015).

