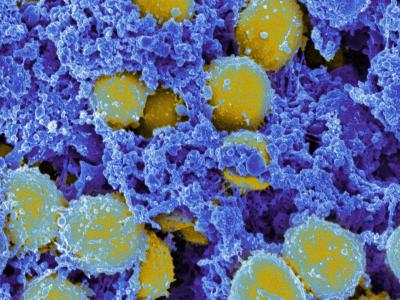
Scanning electron micrograph of Staphylococcus aureus bacteria.
The skin of people with atopic dermatitis lacks infection-fighting proteins, making them susceptible to skin infections caused by bacteria and viruses. Fungal infections also are common in people with atopic dermatitis.
Bacterial Infections
A major health risk associated with atopic dermatitis is skin colonization or infection by bacteria such as Staphylococcus aureus. Sixty to 90 percent of people with atopic dermatitis are likely to have staph bacteria on their skin. Many eventually develop infection, which worsens the atopic dermatitis.
Viral Infections
People with atopic dermatitis are highly vulnerable to certain viral infections of the skin. For example, if infected with herpes simplex virus, they can develop a severe skin condition called atopic dermatitis with eczema herpeticum.
Those with atopic dermatitis should not receive the currently licensed smallpox vaccine, even if their disease is in remission, because they are at risk of developing a severe infection called eczema vaccinatum. This infection is caused when the live vaccinia virus in the smallpox vaccine reproduces and spreads throughout the body. Furthermore, those in close contact with people who have atopic dermatitis or a history of the disease should not receive the smallpox vaccine because of the risk of transmitting the live vaccine virus to the person with atopic dermatitis.



