This blog is the fifth in a series about the future of NIAID's HIV clinical research enterprise. For more information, please visit the HIV Clinical Research Enterprise page.
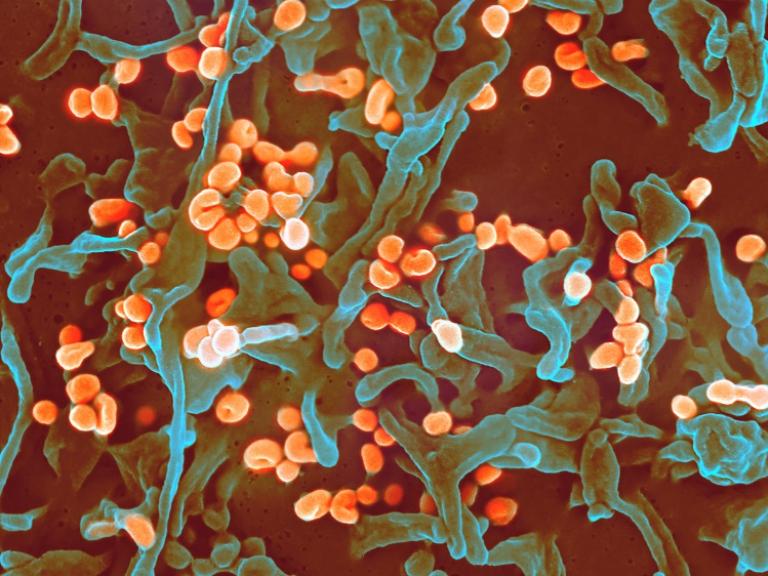
The outcomes of HIV clinical trials are often determined by precisely and accurately measuring how specific interventions work biologically in people. Whether tracking immune responses to a preventive vaccine candidate, monitoring changes to the amount of virus in the body, or screening for certain adverse events after administering a novel therapeutic, study teams routinely interact with clinical trial participants to safely obtain, store, transport, and analyze tissue and bodily fluid samples to answer important scientific questions about the impact of an HIV intervention in a laboratory. High quality, reliable laboratory infrastructure is critical to the accuracy and validity of clinical trial results.
More than 150 NIAID-supported laboratories in 20 countries are addressing the diverse scientific programs of the four clinical trials networks in the Institute’s HIV clinical research enterprise. Since the start of HIV clinical research, laboratory capacities have grown in scope to support an increasing number of global clinical trials, emerging complexities in study protocol design and laboratory testing demands and evolving regulatory requirements for research and licensure.
NIAID is engaging research partners, community representatives, and other public health stakeholders in a multidisciplinary evaluation of its HIV clinical trials networks’ progress toward short- and long-term scientific goals. This process assesses knowledge gained since the networks were last awarded in 2020 to identify an essential path forward based on the latest laboratory and clinical evidence. Future NIAID HIV clinical research investments build on the conclusions of these discussions.
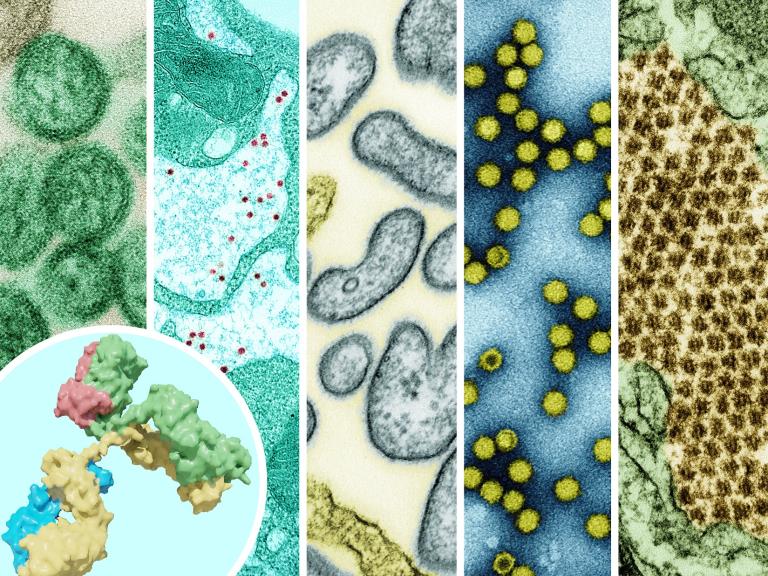
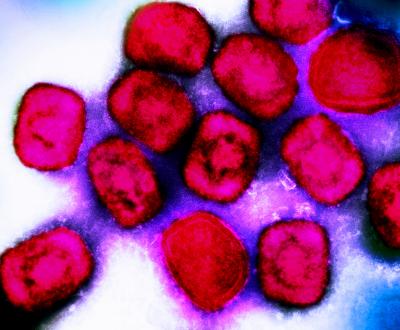
In the next iteration of HIV clinical trials networks, laboratory functions will continue to evolve to align with scientific priorities and research approaches. Networks will support small early-phase trials, large registrational trials and implementation science research to examine preventive vaccine candidates and non-vaccine prevention interventions, antiviral treatments, HIV curative strategies, and therapies to improve the clinical outcomes of people affected by and living with HIV. Selected studies also will rely on high quality laboratory resources to examine interventions for tuberculosis, hepatitis, mpox and other infectious diseases. Clinical trial networks will need to employ a variety of laboratory types to achieve these objectives. To increase flexibility and ensure the timeliness and the high quality standards the HIV field relies on for evidence that informs science, licensure and equitable practice, NIAID will have the ultimate authority for laboratory selection and approval.
Efficiency and Versatility
Laboratory assays for HIV clinical trials continue to expand in quantity and complexity and require proportionate technical expertise and management. Future clinical research needs will include immunologic, microbiologic, and molecular testing, as well as standard chemistries and hematologic assays, with fluctuating volumes across a global collection of research sites. Balancing capacity, efficiency, scalability, and cost will require a mixed methods approach. These may include centralized laboratory testing where feasible and advantageous for protocol-specified tests; standardized processes for rapid assessment and approval of new network laboratories; and validated third-party outsourcing of routine assays to ensure timely turnaround when demands surge.
Quality and Standardization
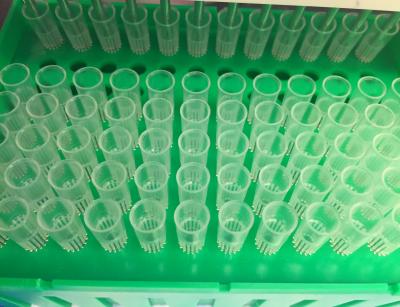
Ensuring consistent laboratory operations and high quality laboratory data will require continued compliance with the NIAID Division of AIDS Good Clinical Laboratory Practices and other applicable regulatory guidelines, ongoing external quality assurance monitoring, strong inventory management, importation and exportation expertise, and data and specimen management.
The research community plays an essential role in shaping NIAID’s scientific direction and research enterprise operations. We want to hear from you. Please share your questions and comments at NextNIAIDHIVNetworks@mail.nih.gov.
About NIAID’s HIV Clinical Trials Networks
The clinical trials networks are supported through grants from NIAID, with co-funding from and scientific partnerships with NIH’s National Institute of Mental Health, National Institute on Drug Abuse, National Institute on Aging, and other NIH institutes and centers. There are four networks—Advancing Clinical Therapeutics Globally for HIV/AIDS and Other Infections, the HIV Vaccine Trials Network, the HIV Prevention Trials Network, and the International Maternal Pediatric Adolescent AIDS Clinical Trials Network.