A major goal of NIAID-supported research on HIV treatment today is to develop long-acting therapies that—unlike current antiretrovirals, which require daily dosing—could be taken only once a week, once a month, or even less often. Such long-acting therapies might be easier for some people to stick to than daily pills, and might also be less toxic and more cost effective. The three types of agents under study are long-acting drugs, broadly neutralizing antibodies, and therapeutic vaccines.
Long-Acting Drugs
NIAID-supported scientists aim to develop a new array of drugs for HIV treatment that include longer-acting pills as well as alternative formulations such as injections, patches, and implants. The complexity of developing such products has led NIAID to create a consortium of experts who can facilitate relationships among the many types of researchers needed to translate an idea for a long-acting HIV drug into a workable solution. Called LEAP, for Long-Acting/Extended Release Antiretroviral Resource Program, the consortium includes scientists and clinicians from academia, industry, and government, as well as patient advocates. Read more about LEAP.
NIAID also will investigate the effectiveness of two investigational long-acting HIV drugs, rilpivirine LA and cabotegravir LA, in people for whom adhering to conventional antiretroviral therapy has been a challenge. Another study is planned to test whether the combination of monthly injections of cabotegravir LA and monthly infusions of an NIAID-discovered broadly neutralizing antibody called VRC01LS can keep HIV suppressed in people whose infection was previously controlled by antiretroviral therapy.
Broadly Neutralizing Antibodies
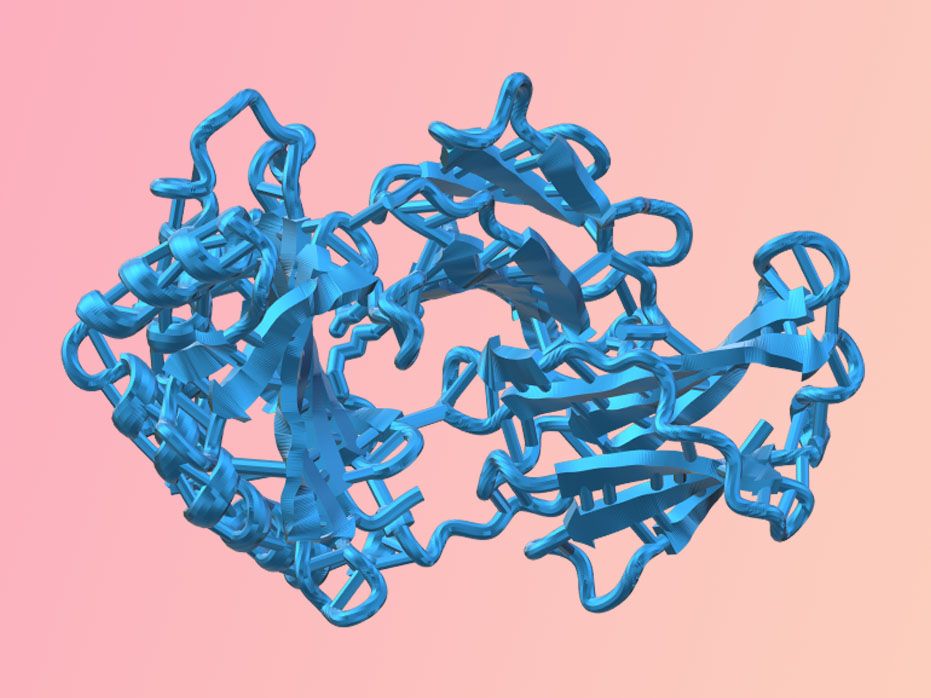
Scientists at the NIAID Vaccine Research Center (VRC) and NIAID-supported scientists at other institutions are developing and testing multiple antibodies for the treatment of HIV. Antibodies are good candidates for treatment because they have few side effects and can be modified to ensure they last a long time in the body, suggesting that dosing could be every other month or even less often. Importantly, the antibodies under investigation can powerfully stop a wide range of HIV strains from infecting human cells in the laboratory and thus are known as broadly neutralizing antibodies, or bNAbs.
In the context of treatment, bNAbs can potentially thwart HIV in three ways:
- By binding directly to the virus, preventing it from entering a cell and accelerating its elimination.
- By binding to an HIV-infected cell, recruiting immune-system components that facilitate cell killing.
- By binding to a key fragment of HIV, forming a complex that may lead to the stimulation of immune cells in a manner similar to a vaccine, thereby preparing the immune system for future encounters with the virus.
Clinical studies have established that giving infusions of certain bNAbs to people living with HIV can suppress the virus, albeit to a limited degree. Further studies have shown that treating people living with HIV with just one bNAb fosters the emergence of HIV strains that are resistant to the antibody. Thus, just as antiretroviral therapy requires a combination of drugs to effectively suppress HIV, it appears that antibody-based therapy will require a combination of either multiple bNAbs or bNAbs and long-acting drugs to suppress the virus. Studies in monkeys infected with a simian version of HIV have already demonstrated that combinations of complementary bNAbs powerfully suppress the virus for an extended period. NIAID is now funding and conducting clinical trials of this strategy for treating HIV in people.
In addition, scientists are engineering changes to known bNAbs to optimize them for HIV treatment and prevention applications. These changes are designed to increase the number of HIV strains an antibody can block, how long the antibody lasts in the body, how powerfully the antibody attaches to the virus, and how efficiently the antibody triggers the immune system to attack both the virus and HIV-infected cells.
Therapeutic HIV Vaccines
Perhaps the ideal treatment for HIV infection would be a therapeutic vaccine. Unlike a vaccine designed to prevent HIV infection, a therapeutic vaccine would be given to people already infected with the virus. Such a vaccine would stimulate the immune system to be ready to control any future emergence of HIV and thereby end the need for further therapy, perhaps save periodic booster shots. Such an approach could lead to sustained viral remission, meaning treatment or vaccination that would result in prolonged undetectable levels of HIV without regular antiretroviral therapy.
The presence of rare people living with HIV who can control the virus naturally either from the time of infection or after halting antiretroviral therapy is evidence that a therapeutic vaccine could theoretically alter the immune system to achieve long-term control of HIV. Nevertheless, attempts to create effective therapeutic HIV vaccines have so far been unsuccessful. To help improve results, NIAID is working to advance the underlying science—in particular, to improve understanding of immune responses that sustainably suppress HIV and to improve the potency of those responses.
Three of the NIAID-funded Martin Delaney Collaboratories are pursuing strategies that involve therapeutic vaccines to achieve long-term control of HIV or reduction of the reservoir of all virus-carrying cells. Read more about the Martin Delaney Collaboratories.
Future Directions for Developing Daily HIV Drugs
At the same time, NIAID continues to support research to develop new drugs with unique mechanisms of action for daily antiretroviral therapy. Such drugs likely would be effective against HIV strains with resistance to other drug types.
For example, basic NIAID-supported research contributed to development of the experimental drug islatravir (also known as EFdA or MK-8591), which belongs to a class of drugs known as nucleoside reverse transcriptase translocation inhibitors, or NRTTIs. NIAID research also contributed to the development of maturation inhibitors, investigational drugs that target the same stage of the HIV lifecycle as protease inhibitors but act by a different mechanism.
Researchers also are attempting to target other parts of the HIV lifecycle. For example, the experimental inhibitor fostemsavir blocks HIV from infecting immune cells by attaching to the gp120 protein on the virus’ surface. Another example is development of capsid assembly inhibitors, which halt construction of the viral capsid, the protein shell that encloses HIV’s genetic material.
For more information on investigational antiretroviral treatments, see the AIDSinfo Drug Database.
Scientific Advances
Effects of Modified Anti-HIV Broadly Neutralizing Monoclonal Antibodies
August 29, 2024NIAID scientists examined the effects of modified anti-HIV broadly neutralizing antibodies (bNAbs) that have an increased ability to bind to cells in the body at a region called the Fc receptor.