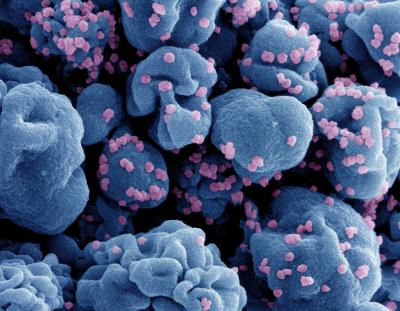
Colorized scanning electron micrograph of a cell (blue) infected with the Omicron strain of SARS-CoV-2 virus particles (pink), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland.
SARS-CoV-2 may have both immediate and long-term symptoms associated with infection. According to the Center for Disease Control and Prevention, 7.5% of U.S. adults develop post-acute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID. PASC is characterized by varying symptoms, including fatigue, shortness of breath, heart palpitations or chest pain, brain fog, insomnia, dizziness, and joint or muscle pain. These symptoms begin around 4 weeks after initial infection with SARS-CoV-2 and can persist for weeks or months after onset. Previous studies have examined the epidemiology of PASC utilizing questionnaire or electronic medical records data, focusing primarily on prevalence of symptoms and healthcare utilization. However, few studies to date have examined potential risk factors for PASC or potential diagnostic data (beyond symptomology) from PASC patients.
To address this need, NIAID scientists initiated a longitudinal cohort study to identify risk factors for PASC and to characterize persistent symptoms following COVID-19 recovery. Adults with a recent documented SARS-CoV-2 infection, either asymptomatic or symptomatic, and those with no history of SARS-CoV-2 infection were enrolled for participation. Upon enrollment, participants underwent a comprehensive evaluation of their past medical history and their current physical and mental health. Blood samples were also collected at this initial visit to measure multiple diagnostic endpoints, including immunologic factors, antibodies, and immunoglobulins. While enrollment into this study is still ongoing, data from the first 309 participants enrolled have been reported to potentially inform treatment decisions for those affected more broadly.
Despite a large majority (88%) of the study participants in the COVID-19 group not requiring hospitalization, 55% of the COVID-19 group reported 1 or more PASC-related symptoms. Women or individuals with a self-reported history of an anxiety disorder had a significantly increased risk of developing PASC symptoms. Further, individuals with PASC had significantly reduced health-related quality of life compared to those without PASC. There was no evidence of viral infection, abnormal immune activation, or autoimmunity in participants with PASC. These findings suggest an increased physical and mental burden on already heavily burdened populations following COVID-19, highlighting the importance to continue studying PASC to better understand pathogenesis, prevention, and treatment.
Reference: Sneller MC, et al. A Longitudinal Study of COVID-19 Sequelae and Immunity: Baseline Findings. Ann Intern Med. 2022 Jul;175(7):969-979. doi: 10.7326/M21-4905. Epub 2022 May 24. PMID: 35605238


