The Immune Mechanisms of Protection Against Mycobacterium tuberculosis Centers (IMPAc-TB) program, established by NIAID in 2019, aims to elucidate the immune responses essential for protecting people against infection with Mycobacterium tuberculosis (Mtb). This program will lead to a better understanding of tuberculosis (TB) immunology, which is critical to guide the design and development of new and improved TB vaccines. The program aligns with the goals and objectives of the NIAID Strategic Plan for Tuberculosis Research.
Main Areas of Focus
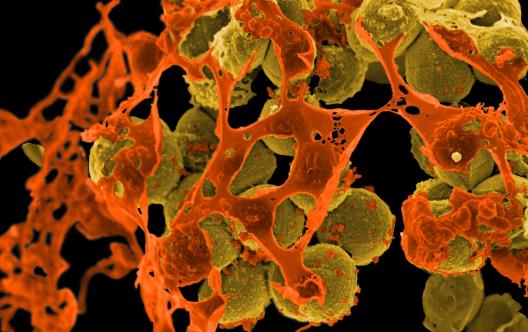
The IMPAc-TB program aims to develop a comprehensive understanding of the immune responses required to prevent initial infection with Mtb, the establishment of latent infection, and transition to active TB disease. To accomplish these objectives, multidisciplinary research teams conduct immunological analyses of tissue-specific and systemic responses using human samples, combined with assessments using small animals, non-human primates (NHPs) and computational modeling. These integrated approaches are designed to identify the key immune responses needed for protection against Mtb; determine immunologic targets that can be used to improve TB vaccine strategies; determine the impact of human immunodeficiency virus (HIV) and nontuberculous mycobacteria (NTM) infections on relevant immune responses to Mtb infection or TB vaccines; and identify how bacterial immune evasion mechanisms subvert immune responses to Mtb.
Locations
Harvard T.H. Chan School of Public Health, Boston
Principal investigators: Sarah Fortune, M.D. (Harvard); Henry Boom, M.D. (Case Western Reserve University, Cleveland); JoAnne Flynn, Ph.D. (University of Pittsburgh)
Center objective: The goal of this Center is to identify factors that protect people from Mtb infection and to translate these findings into improved vaccine strategies. A multidisciplinary research team assesses samples from NHPs and human cohorts, in whom infection is suppressed, to learn how their immune responses protect them from Mtb infection. Investigators use computational modeling to predict the likely causes of suppressed infections, which is being tested in cellular and small animal models. Studies evaluate the effect of intravenous (IV) Bacille Calmette-Guerin (BCG) vaccination in rhesus macaques in response to Mtb challenge and the immune mechanisms responsible for controlling natural mycobacterial infection in cynomolgus macaques. Studies also examine the effect of Simian Immunodeficiency Virus/SIV infection on IV BCG vaccination using computational modeling and a systems biology approaches. Also, the research team compares the immune correlates of protection observed in the NHP studies with human responses. Human studies conducted by the Center also will also focus on exposed individuals that resist infection or that develop a transient infection response.
Seattle Children's Hospital
Principal investigator: Rhea Coler, Ph.D.
Center objective: This Center will identify the complex immune responses required to prevent Mtb infection or active TB disease by comparing and examining protective immune responses induced by natural mycobacterial infection or vaccines. The research team evaluates recombinant protein vaccines combined with adjuvants to identify and validate common protective correlates of immunity in well-established animal models for TB and human challenge clinical studies where participants are deliberately exposed to BCG (as a controlled human infection model) under carefully controlled conditions. The investigational vaccines being evaluated are ID93 and M72 formulated with GLA-SE and other adjuvants developed by Access to Advanced Health Institute (AAHI) and contractors supported by NIAID’s Division of Allergy, Immunology, and Transplantation’s (DAIT) adjuvant program. The studies also address how immunity from previous BCG vaccination and natural nontuberculous mycobacteria (NTM) infection affects the investigational vaccines’ effectiveness and ability to generate an immune response across species. The studies will provide crucial insights into the development of candidate vaccines that generate robust levels of durable, protective immunity against TB.
Seattle Children’s Hospital
Principal investigator: Kevin Urdahl, M.D., Ph.D.
Center objective: The goal of this Center is to inform the design of an effective TB vaccine by identifying the immune responses capable of controlling and potentially eradicating Mtb. The research team is identifying and examining protective pathways in natural and vaccine-induced immunity by analyzing tissue-specific and systemic immunity in mice, NHPs, and humans. Investigators are focusing on immune correlates at three stages: the pre-infection immune stage; the early events after pulmonary infection; and the formation of granulomas (compact, organized structures of immune cells) during chronic infection. These studies will identify the immune responses required to protect the host from initial infection, establish latent infection, and prevent progression to active TB disease.
Contact Information
Dr. Que Dang, Division of AIDS (DAIDS)
Dr. Nancy Vázquez, Division of Allergy, Immunology, and Transplantation (DAIT)
Dr. Katrin Eichelberg, Division of Microbiology and Infectious Diseases (DMID)
Dang Q et al. Immune mechanisms of protection against Mycobacterium tuberculosis-centers. 2024 Oct 8:15:1429250. doi: 10.3389/fimmu.2024.1429250. eCollection 2024.
STAT3 dominant-negative disease (STAT3DN)—also known as autosomal dominant hyper-IgE syndrome (AD-HIES) or Job’s Syndrome—results from mutations in the gene that encodes a signaling protein called STAT3. People with this disease tend to have very high levels of an antibody called immunoglobulin E (IgE), recurrent infections of the skin and lungs, recurrent bone fractures, unusually flexible joints, and inflamed skin.
STAT3 dominant-negative disease has widespread deleterious effects on patients’ health, so NIAID scientists aim to develop and enhance treatments to improve patients’ quality of life. In addition, NIAID scientists hope that studying this disease will help them better understand the physiological processes associated with the genetic tendency to develop certain types of infections and allergic diseases.
NIAID investigators identified the role of STAT3 in this disease in 2007. Since then, NIAID-supported researchers have made multiple discoveries about how the loss-of-function mutation in the STAT3 gene leads to patients’ symptoms. NIAID-supported clinical research seeks to determine the effect of STAT3 dominant-negative disease on the immune system, including which immune cells and responses are affected and how these abnormalities translate into patients’ symptoms.
Causes
STAT3 dominant-negative disease results from mutations in the gene that encodes a signaling protein called STAT3. This protein is involved in many different activities of the body, explaining why the disease affects not only the immune system but also facial appearance, bones, lungs, skin, and arteries.
Signs and Symptoms
People with STAT3 dominant-negative disease (STAT3DN) have very high levels of IgE and may have recurrent infections of the skin and lungs. These infections are often caused by the bacterium Staphylococcus aureus but also may be caused by other bacteria and fungi. Patients also tend to have recurrent bone fractures, unusually flexible joints, and inflamed skin, and may have a rash similar to eczema. Baby teeth in people with this disease often do not fall out on their own. People with STAT3DN also often have distinctive facial characteristics, such as uneven facial features, prominent forehead, deep-set eyes, broad nasal bridge, wide, fleshy nose tip, and protruding lower jaw.
In 2008, NIAID scientists discovered that important immune cells called Th17 cells are missing in people with STAT3DN. NIAID researchers also found in 2011 that an unusually low number of immune memory cells may cause people with the disease to be more susceptible to some viral infections. In 2013 and 2016, NIAID researchers showed that the STAT3 mutation protects people from more severe allergic disease by interfering with the process that causes typical allergic reactions.
Diagnosis
A doctor will suspect STAT3DN in a person with eczema, very high IgE, recurrent boils, and pneumonias. Blood tests diagnosing the disease will show normal levels of IgG, IgA, and IgM antibodies but very high levels of IgE antibodies. People with the disease also may show a high number of white blood cells called eosinophils and a poor response to immunizations. Sequencing of the patient’s DNA can confirm the presence of the STAT3 mutation.
Treatment
The most effective treatments for STAT3 dominant-negative disease are continuous antibiotics and antifungals as needed, as well as careful monitoring for infections, which can be severe even when symptoms do not appear so. Some patients receive antibody replacement therapy. Antiseptic approaches, such as dilute bleach baths, often help prevent skin infections and improve eczema.
Disease-Specific Vaccines
NIAID supports and conducts research to identify new vaccine candidates to prevent a variety of infectious diseases, including those for which no vaccines currently exist. NIAID-supported research also aims to improve the safety and efficacy of existing vaccines. Explore the links below to learn more about NIAID’s efforts to design, develop and evaluate new and improved vaccines to protect against specific infectious diseases.
Allergy, Immunology & Transplantation
Immcantation Portal
The Immcantation framework is developed as a start-to-finish analytical ecosystem for large-scale characterization of B cell receptor (BCR) and T cell receptor (TCR) repertoires from high-throughput adaptive immune receptor repertoire sequencing (AIRR-seq) datasets. Immcantation provides Python and R packages for pre-processing of raw sequencing reads, population structure determination, and repertoire analysis.
Asthma Risk Factors and Prevention Research
Understanding Asthma Triggers
Managing Asthma Symptoms
QuSAGE—Quantitative Set Analysis for Gene Expression
This Gene Set Enrichment-type test designed for analysis of microarray and RNASeq data is designed to provide a faster, more accurate, and easier to understand test for gene expression studies. QuSAGE extends previous methods with a complete probability density function (PDF). From this PDF, P values and confidence intervals can be easily extracted.

