This blog is adapted and cross-posted from HIV.gov.
During the first full day of presentations at the 2024 Conference on Retroviruses and Opportunistic Infections (CROI), HIV.gov spoke with Carl Dieffenbach, Ph.D., director of NIAID’s Division of AIDS, about research presented on Doxy-PEP for sexually transmitted infections (STIs) and HIV vaccines. He spoke with Louis Shackelford of the HIV Vaccine Trials Network. Watch their conversation.
Louis also spoke with LaRon Nelson, Ph.D., R.N., F.N.P., F.N.A.P., F.N.Y.A.M., F.A.A., about community-engaged research, HIV prevention at CROI, and a new study (HPTN 096) he is leading to reduce HIV rates among Black men who have sex with men (inclusive of cisgender and transgender men) in the southern United States. Dr. Nelson is a professor and the associate dean at the Yale School of Nursing. Watch their conversation.
Insights from Doxy-PEP Use in Real World Settings
At last year’s CROI, researchers presented results from an NIH-supported study on using a preventive dose of the antibiotic doxycycline as post-exposure prophylaxis within 72 hours after condomless sex to prevent bacterial STIs, an approach that has become known as Doxy-PEP. (View last year’s Doxy-PEP discussion with Dr. Dieffenbach.) Here at CROI 2024, Dr. Annie Luetkemeyer of the University of California, San Francisco, shared additional findings from the open-label extension of that original study, which found sustained reduction of bacterial STIs among men who have sex with men and transgender women living with HIV or on PrEP in Seattle and San Francisco. The San Francisco AIDS Foundation (SFAF) was one of the first organizations in the United States to roll out Doxy-PEP, beginning in late 2022 when it was offered to all active PrEP clients at their visits at the Magnet clinic. SFAF medical director Dr. Hyman Scott reported that there was high uptake among clients and that bacterial STIs decreased by nearly 60% in less than a year at SFAF’s clinic. The decline was highest for syphilis (78%) and chlamydia (67%).
The San Francisco Department of Public Health (SFDPH) presented the first findings to measure the effect of Doxy-PEP at the population level. Their analysis, presented by epidemiologist Madeline Sankaran, showed a substantial and sustained decline in the number of chlamydia and early syphilis infections in San Francisco among men who have sex with men and transgender women over the 13 months after the Department released guidelines for the use of Doxy-PEP. As in the other studies presented, SFDPH did not see corresponding significant declines in gonorrhea. Doxy-PEP is not recommended for cis-gender women because there is not yet evidence to suggest it is effective for them.
HIV Vaccine Trials Continue
Dr. Dieffenbach also discussed ongoing research to find a vaccine to prevent HIV, the topic of several presentations at the conference so far. Since there are a number of Phase I HIV vaccine trials currently underway, he and Louis spoke about what those smaller trials do. Then they discussed what some of the HIV vaccine trials currently underway are exploring.
Other Studies of Interest Presented on Monday
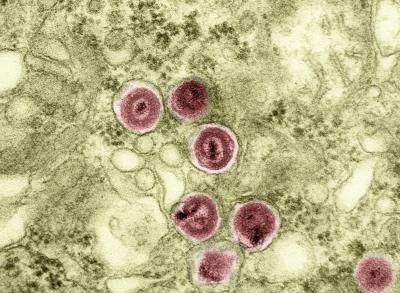
Some of the other studies presented centered on broadly neutralizing antibodies (bNAbs), including bNAbs as part of HIV therapy and how different HIV variants can affect bNAb efficacy as a treatment method. A new analysis from the pivotal HVTN 083 study of long-acting PrEP with cabotegravir found no significant risk of hypertension in people using the method, which had been a concern in some previous clinical studies of the same class of antiretroviral drugs.
Community-Engaged Research
The importance and significant benefits of involving community in all aspects of HIV research was the first topic Dr. Nelson and Louis discussed. “If we don’t have community voices or engaged communities, we aren’t going to be asking the right questions or designing the studies in the best ways that will produce the outcome that we need, and we won’t end up with answers that are as relevant as they could be,” Dr. Nelson observed. He pointed to the dapivirine vaginal ring as an example of better outcomes because communities were involved in research. He said he hopes that community engagement in research continues to become more and more common, but it requires that researchers be willing to listen and, when needed, change their plans based on what they hear from community.
HIV Prevention Research at CROI
Dr. Nelson highlighted some of the HIV prevention topics at CROI that have caught his attention, such as increasing equitable use of long-acting injectable forms of HIV PrEP and treatment among different populations and in different countries. Other discussions of interest have included early studies on potentially very long-acting forms of HIV PrEP and exploration of possible dual prevention tools that would provide users with both HIV PrEP and contraception.
HPTN 096 Study
Finally, Dr. Nelson discussed an example of community-informed research that will soon be underway: the NIH-supported study through the HIV Prevention Trials Network (HPTN) known as HPTN 096. It aims to reduce HIV rates among Black men who have sex with men in the southern United States using a strategy developed based on what communities have told Dr. Nelson and colleagues is needed to do so. As a result, the study includes a package of four interventions which simultaneously address social, structural, institutional, and behavioral barriers to HIV prevention and care. HPTN 096 will soon launch in Atlanta, south Florida, Montgomery, Memphis, and Dallas.
More HIV Research Updates to Follow on HIV.gov
HIV.gov will be sharing additional video interviews from CROI 2024 with Dr. Dieffenbach, CDC’s Dr. Jono Mermin and Dr. Robyn Neblett Fanfair, and others. You can find all of them on HIV.gov’s social media channels and recapped here on the blog.