This blog is adapted and cross-posted from HIV.gov.
On March 6 as the 2024 Conference on Retroviruses and Opportunistic Infections (CROI) was winding down, HIV.gov spoke with Carl Dieffenbach, Ph.D., director of NIAID's Division of AIDS, about highlights of long-acting HIV treatment research discussed at the conference. He spoke with Brian Minalga, M.S.W., deputy director of the NIH-supported Office of HIV/AIDS Network Coordination. Watch their conversation below:
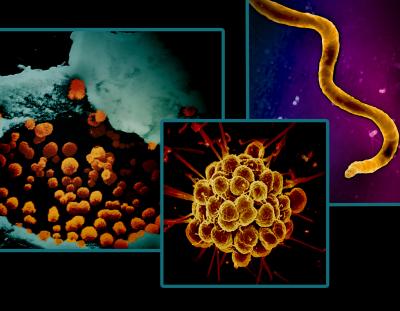
Research Suggests Possible Expanded Options for Long-Acting HIV Treatment
Dr. Dieffenbach highlighted findings from several clinical trials and a plenary session presented at CROI about current and future options for long-acting antiretroviral treatment (ART) for HIV.
First, he discussed a NIAID-supported randomized clinical trial that found that long-acting ART with cabotegravir and rilpivirine was superior in suppressing HIV replication compared to daily oral ART in adults who had been unable to maintain viral suppression through an oral daily regimen. The LATITUDE study enrolled participants in 31 sites in the United States. Last month, the trial’s Data and Safety Monitoring Board conducted a planned review of interim data and recommended halting randomization and offering all eligible study participants long-acting ART based on its observed superior viral suppression of HIV. At CROI, study leaders reported that the interim analysis of data from 294 participants showed that the chance of experiencing unsuppressed HIV was 7% among people taking long-acting ART compared to 25% among those taking daily oral ART. The likelihood of discontinuing the assigned regimen due to adverse events or experiencing unsuppressed HIV was 10% among people taking long-acting ART compared to 26% among those taking daily ART. These findings were statistically significant. Dr. Dieffenbach observed that these results may support expanding the use of long-acting ART among a broader population. Read the study abstract. Read more in this NIAID news release.
Another ongoing clinical trial reported initial findings on the safety of the same long-acting injectable treatment regimen for adolescents with HIV with a suppressed viral load. The NIH-supported MOCHA study enrolled participants aged 12 to 17 who were virally suppressed in Botswana, South Africa, Thailand, Uganda, and the United States. In what he characterized as very encouraging results, Aditya Gaur, M.D. of St. Jude Children's Research Hospital, one of the trial’s co-chairs, reported that after the first six months all participants remained virally suppressed, and the level of the ART in their systems was comparable to what has been shown as efficacious in adult studies of the same drug. He also reported that, while about one-third of the participants reported an injection-site reaction, there were no surprising or unanticipated adverse events. These data support the use of cabotegravir and rilpivirine in virally suppressed adolescents, according to Dr. Gaur and colleagues. Dr. Dieffenbach noted that NIH will continue to support safety and dosing studies to determine the proper doses for adolescents and that these studies could eventually expand access to this long-acting HIV treatment to more people.
Read the abstract. Read NIAID’s news release about the study.
In addition, Dr. Dieffenbach mentioned an industry-sponsored Phase 2 trial that presented 24-week results of an oral once-weekly investigational combination of two drugs (islatravir and lenacapavir). Researchers reported that the investigational combination maintained a high level of viral suppression among study participants and was well tolerated. The study will continue to gather data and suggests that a weekly oral HIV treatment regimen could someday be possible. Read the abstract.
Finally, Dr. Dieffenbach discussed Wednesday’s plenary session by Charles Flexner, M.D. of The Johns Hopkins University School of Medicine, which was titled “The End of Oral? How Long-Acting Formulations Are Changing the Management of Infectious Diseases.” In his big picture, future-focused presentation exploring long-acting drug delivery, Dr. Flexner observed that there is a need for HIV products with less frequent dosing, greater convenience, and greater likelihood of viral suppression, as well as for the prevention and treatment of other diseases, including tuberculosis, malaria, and viral hepatitis. He discussed recent advances in formulation science that are going to help make available better replacements for daily oral drugs for HIV and many other infectious diseases. Dr. Dieffenbach underscored Dr. Flexner’s point that these novel products must be developed with access and equity in mind so that people who need them, especially in resource-limited settings, can use them.
Key Takeaways
Reflecting on key takeaways from the entire conference, both Dr. Dieffenbach and Brian pointed to the importance of partnership between the HIV community and scientists in all aspects of HIV research, a theme also discussed in HIV.gov’s conversation with Dr. LaRon Nelson from the conference. In terms of research highlights, Dr. Dieffenbach pointed to the results reported from the IMPAACT P1115 study in which several children who started HIV treatment within hours of birth later surpassed a year of HIV remission after a treatment pause. (See HIV.gov’s interview with Dr. Deborah Persaud about this study.) He also noted that the additional data accumulating on the effectiveness of Doxy-PEP is encouraging and will hopefully soon be reflected in clinical guidelines that help to reduce the incidence of syphilis, chlamydia, and gonorrhea in men who have sex with men and transgender women.
Catch Up on More HIV Research Updates
HIV.gov has shared other interviews from CROI 2024 with federal HIV leaders, participating researchers, and community members. You can find all of them on HIV.gov’s blog and social media channels.
About CROI
More than 3,600 HIV and infectious disease researchers from 73 countries gathered in Denver and virtually from March 3-6 this year for CROI, an annual scientific meeting on the latest research that can help accelerate global progress in the response to HIV and other infectious diseases, including STIs and viral hepatitis. Over 1,000 summaries of original research were presented. Visit the conference Web site for more information. Session webcasts and more information will be published there for public access.