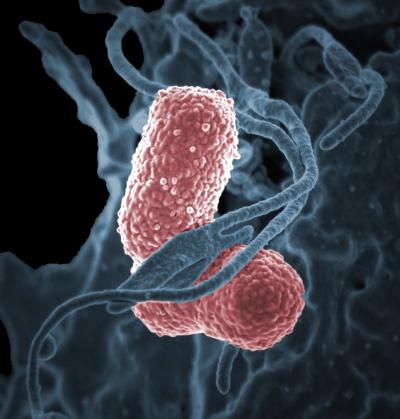
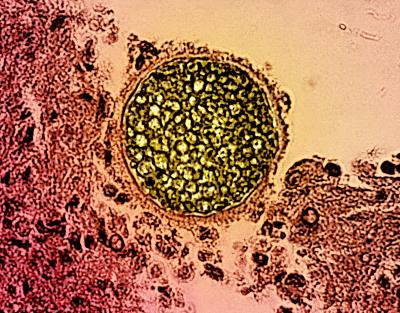
Help advance phage therapy research to fight antibiotic resistance (AR) by applying to the Centers for Accelerating Phage (Bacteriophage) Therapy to Combat ESKAPE Pathogens (CAPT-CEP) (P01, Clinical Trial Not Allowed) notice of funding opportunity (NOFO). Specifically, the aim of this research is to combat ESKAPE pathogens—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.—that are among the top ten pathogens attributed to AR deaths. This initiative aims to fill the gaps in phage therapeutics research and development (R&D), and thus contribute to the fight against AR.
Research Objectives and Scope
The objective of this NOFO is to establish collaborative, multidisciplinary research groups that will implement phage therapeutic research and facilitate interactions within and among teams of researchers from diverse scientific fields. The major goals of the CAPT-CEPs will be to 1) develop novel, high-throughput, and cutting-edge assays, tools, and models for phage therapy that can be applied to other phage R&D studies and 2) perform essential studies to understand pharmacokinetics and pharmacodynamics (PKs/PDs) and evaluate optimal delivery systems and dosages of phages, which can be used in designing future clinical trials to combat ESKAPE pathogens.
Applications must focus on the preclinical development of phage therapies that target at least one of the ESKAPE pathogens listed above. Academic institutions are encouraged to include a substantive investment and participation in the project by an industry participant to facilitate appropriate and validated product development activities.
Overarching themes could include, but are not limited to:
- Developing assays, tools, and models, including in silico, in vitro, and in vivo, to help standardize phage therapy R&D.
- Generating suitable in vitro and in vivo models for phage research against ESKAPE pathogens.
- Understanding PK/PD relationships for phages.
- Determining (poly)valency, delivery routes, and dosages of different phage products.
Refer to the NOFO for a list of multidisciplinary research projects that could contribute to those unifying themes.
Keep in mind, NIAID will consider applications proposing research in the areas listed below to be nonresponsive and not review them:
- Projects that do not target at least one ESKAPE pathogen—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter.
- Basic science that does not support development of phage therapeutics.
- Decolonization-focused studies.
- Wound infection studies.
- Mycobacteria or drug-resistant tuberculosis.
- Clinical trials as defined by the NIH; however, the use of existing clinical samples is permitted.
Overall CAPT-CEP Structure
The CAPT-CEP should be organized around a common research theme to establish a multidisciplinary team. The required components are an Administrative Core and a minimum of two, but no more than three, synergistic Research Projects organized around the common theme; up to two Scientific Cores are optional.
Application Requirements
NIAID will fund two or three Centers in fiscal year 2026.
Application budgets are not expected to exceed $1.2 million in annual direct costs. The scope of the project should determine the project period, with a maximum project period of 5 years.
Applications are due January 28, 2025, by 5 p.m. local time of the applicant organization.
Direct any scientific/research questions to Dr. Kyung Moon at kyung.moon@nih.gov or 240-669-5515. For questions about peer review, contact Dr. Soheyla Saadi at saadisoh@nih.gov or 240-669-5178.