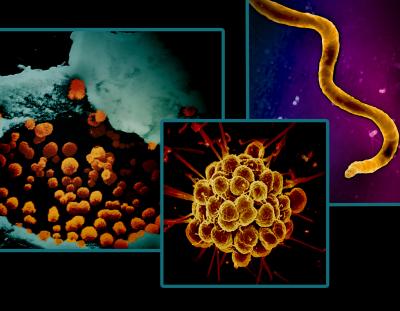
Sexually transmitted infections (STIs) are caused by bacteria, viruses, or parasites. STIs have a devastating impact on adults and infants and annually affect millions of people in the United States. Certain STIs can increase a person’s risk of developing cancer and increase the likelihood of acquiring or transmitting HIV. In addition, STIs can cause long-term health complications, especially in the reproductive and central nervous systems. In rare cases, they can lead to serious illness or death.
NIAID supports research across the spectrum from basic to clinical science to develop effective diagnostic, preventive and therapeutic approaches to STIs in alignment with the National STI Strategic Plan. In recognition of National STI Awareness Week, NIAID shares a snapshot of new projects and recent scientific advances in STI research.
Improving treatment for syphilis and trichomoniasis
New reports of syphilis and congenital syphilis are increasing at an alarming rate in the United States. Syphilis is caused by the bacterium Treponema pallidum. Benzathine penicillin G (BPG) is one of only a few antibiotics known to effectively treat syphilis. There is currently a shortage of BPG, and some people are allergic to penicillin antibiotics. In February 2024, NIAID convened a workshop with a wide range of experts on alternative therapies to BPG for the treatment of adult syphilis, neurosyphilis, and syphilis in pregnant persons and infants. The workshop addressed preclinical evaluation of candidate drugs, the potential need for studies on how candidate drugs are processed in the body during pregnancy, and how to approach clinical trials of treatment for congenital syphilis. This work is part of NIAID’s comprehensive portfolio of syphilis diagnosis, prevention, and treatment research.
Trichomoniasis is the most common parasitic STI, caused by Trichomonas vaginalis. Trichomoniasis can increase the risk of getting or spreading other STIs, including HIV. The parasite can also cause inflammation of the cervix and the urethra. T. vaginalis is treated with an antibiotic drug class called nitroimidazoles. The currently recommended nitroimidazole, called metronidazole, cures 84-98% of T. vaginalis cases but does have high rates of breakthrough infection. A new project led by Tulane University will examine a single dose of secnidazole, a medicine in the same drug class, as a more effective and cost-effective treatment option for women and men.
Developing a vaccine for herpes simplex virus 2
Herpes simplex virus 2 (HSV-2) is a common subtype of herpes simplex virus that is transmitted through sexual contact. The Centers for Disease Control and Prevention estimates that 18.6 million people aged 15 years and older United States live with HSV-2. In severe cases, HSV-2 may lead to life-threatening or long-term complications. There is no licensed preventive HSV-2 vaccine, and there is no cure. A new project led by the University of Pennsylvania seeks to define correlates of protection for HSV-2, meaning they intend to identify immune processes involved in preventing HSV-2 disease. They will do this by analyzing laboratory samples from animal studies of a promising preventive vaccine candidate that they developed with prior funding. That vaccine candidate is also now in an industry-sponsored early-stage clinical trial. The same project will expand on the HSV-2 targets in the preventive vaccine to develop a therapeutic vaccine concept to reduce recurrent outbreaks. This research responds to the scientific priorities in the NIH Strategic Plan for Herpes Simplex Virus Research.
Increasing fundamental knowledge of bacterial vaginosis
Bacterial vaginosis (BV) results from an imbalance in the vaginal microbiome. BV can be caused by sexual activity, douches and menstrual products. BV can increase women’s biological susceptibility to HIV and other STIs and can cause premature birth or low birthweight if untreated in pregnant people. In a recent publication, NIAID-supported researchers, led by researchers at the University of Washington and University of California San Diego, shared findings on how damage to the vaginal skin barrier occurs during bacterial vaginosis. Those skin barrier cells, called epithelial cells, are covered in carbohydrate molecules called glycans. The research team found that people with BV had damaged glycans on their vaginal epithelial cells. They suggested that future work should examine the relationship between treatment and restoration of normal glycans. If an association is detected, it could help healthcare providers monitor for successful treatment outcomes to reduce the likelihood that BV will return after a course of treatment. The findings were published in Science Translational Medicine.
These activities are among the research investments in NIAID’s STI portfolio. For more information on STIs, please visit: