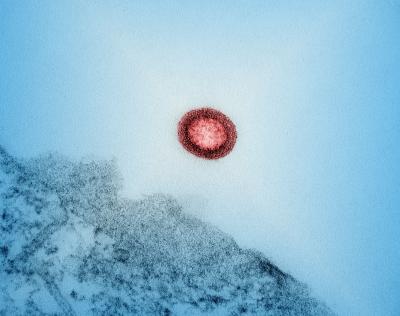
Switching to an antiretroviral therapy (ART) regimen containing the drug dolutegravir was associated with a significant temporary increase in reservoirs of latent HIV, according to a new analysis from a study in Uganda. HIV reservoirs are cells where HIV lies dormant and cannot be reached by the immune system or ART. They are central to HIV’s persistence, preventing current treatments from clearing the virus from the body. The findings were published today in eBioMedicine.
When taken as prescribed, ART can stop HIV from replicating. The different classes of available antiretroviral drugs (ARVs) interrupt different stages of HIV replication. People are often prescribed drug regimens composed of multiple drug classes to increase the likelihood that ART will fully suppress HIV replication. In 2018, many countries began using dolutegravir-based ART regimens following studies that showed the drug had higher efficacy and fewer side effects than the drugs that had been in use previously. Uganda was among these countries and recommended dolutegravir together with the ARVs tenofovir and lamivudine for all people whose HIV was treatable with those drugs.
In 2015, NIH scientists and researchers from the Rakai Health Sciences Program in Uganda began a longitudinal study of reservoirs among people with HIV in the Rakai and Kyotera Districts in Uganda. Study participants were people whose HIV was suppressed by ART and had agreed to provide blood samples and receive a routine physical examination annually. People meeting study entry criteria continued to enroll each year. As part of this study, the team examined whether the introduction of dolutegravir-based regimens in 2018 had any effect on the makeup of HIV reservoirs in study participants. At the time of the published analysis, 63% of participants were female. The study observed that HIV reservoir size was generally decreasing as participants remained virally suppressed for longer periods. In the analysis of samples provided post-dolutegravir introduction, they observed a surprising 1.7-fold average increase in HIV reservoir size above pre-dolutegravir levels, which lasted for approximately a year, then returned to normal. This effect was consistent across the majority of study participants regardless of how long they had been living with HIV.
According to the study authors, no other study has found significant differences in HIV reservoir characteristics due to ART regimen changes, but previous research has identified changes in immune characteristics and cardiovascular disease risk, as well as other effects in the period after dolutegravir initiation, suggesting the body goes through a period of adjustment when switching to use the new drug. The authors state that it is important to explore whether other populations experience the same temporary reservoir increase post-dolutegravir initiation, and that more research is needed to understand the mechanism causing the increase, especially if it is starting dolutegravir or stopping the previous ARV. They further suggest that these findings may inform HIV cure research, including approaches referred to as “Shock and Kill” that attempt to stimulate HIV reservoirs to resume activity, then promptly remove them. The authors did not observe any negative clinical ramifications, such as loss of viral control, associated with this finding.
Most HIV reservoir research has been conducted among predominantly male study populations in Europe and North America, unlike the primarily female participants in this study. The authors highlight the importance of exploring sex-based differences in HIV reservoir characteristics and the inclusion of representative populations in HIV studies.
This research was conducted by NIAID, Western University, and the Rakai Health Sciences Program and with co-funding from other NIH institutes, the Gilead HIV Cure Grants Program, the Canadian Institutes of Health Research, and the Ontario Genomics-Canadian Statistical Sciences Institute.
Reference:
RC Ferreira, et al., Temporary increase in circulating replication-competent latent HIV-infected resting CD4+ T cells after switch to an integrase inhibitor based antiretroviral regimen. eBioMedicine DOI: 10.1016/j.ebiom.2024.105040 (2024)