NIH Trial Gives People with Lupus Data to Inform Treatment Decisions
In people with a form of lupus called systemic lupus erythematosus (SLE), the risk for a severe flare-up of disease was low for both individuals who tapered off long-term immunosuppressive therapy and those who remained on it, a clinical trial has found. The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, sponsored and funded the trial. The findings were reported today in the journal The Lancet Rheumatology.
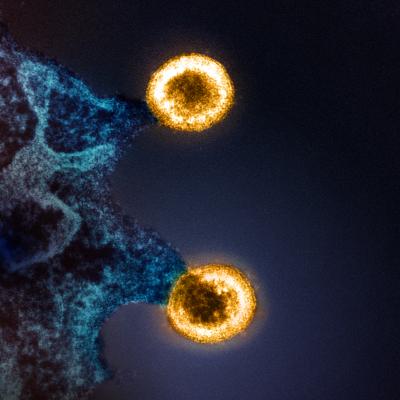
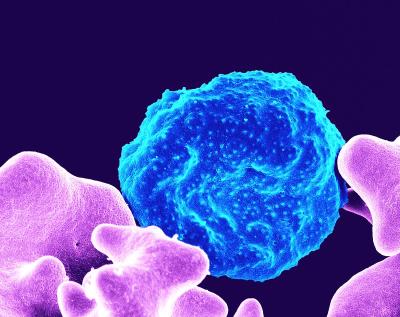
SLE is a chronic autoimmune disease in which the immune system attacks healthy tissues and organs. An estimated 450,000 people in the United States have the disease. Medications that doctors prescribe for people with SLE help suppress or tamp down their overactive immune systems. One of the most prescribed immunosuppressants for SLE, mycophenolate mofetil or MMF, effectively treats moderate and severe forms of the disease but also increases the risk of infections, cancers, severe birth defects, miscarriage, and impaired responses to vaccines when the drug is used long-term. Tapering off MMF once SLE symptoms subside reduces these side effects but could risk exposing the individual to a disease flare with the potential to cause a range of symptoms, including fatigue, rash, arthritis, and internal organ damage.
Until today's report, little evidence existed to help people with SLE and their physicians understand the likelihood of a flare after tapering off MMF. The new findings will help people with SLE make informed decisions about withdrawing treatment based on their personal circumstances and risk tolerance.
The NIAID-funded Autoimmunity Centers of Excellence network conducted the trial under the leadership of Judith A. James, M.D., Ph.D., and Eliza F. Chakravarty, M.D. Dr. James is professor and chair of the Arthritis & Clinical Immunology Research Program at the Oklahoma Medical Research Foundation. Dr. Chakravarty was an associate professor in the same program during the study. The National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of NIH, supports the database for the biological samples processed during the trial.
The trial involved 102 people with SLE ages 18 to 70 whose symptoms had subsided after treatment with MMF. Participants had been taking the drug for an average of 6.6 years. Eighty-four percent of participants were female, reflecting the disproportionate prevalence of lupus in women. Seventy-six percent of participants had a history of lupus nephritis—kidney inflammation that can harm kidney function. Forty-one percent of participants were Black, 40% were White, 21% were Hispanic/Latino, 10% were Asian, and 2% were American Indian/Alaska Native.
The study team assigned participants at random to either taper off MMF over a 12-week period or to remain on their baseline MMF dose. Investigators followed the participants for 60 weeks to monitor if and when they experienced a flare severe or persistent enough to require either new immunosuppressive therapy or higher doses of it.
By week 60, 9 of 51 participants in the MMF withdrawal group and 5 of 49 in the MMF maintenance group had severe or persistent flares requiring new or increased immunosuppressive therapy. The estimated risk of such flares by week 60—a metric that reflected both occurrence and timing—was up to 18% in the withdrawal group and 11% in the maintenance group. The investigators also looked at five different measures of lupus flares and found that treatment withdrawal consistently led to a 6% to 8% increase in the risk for flares. For participants with a history of kidney disease, the increase in risk was higher, at 14%. One benefit of MMF withdrawal, however, was a reduction in infections. Forty-six percent of the withdrawal group had at least one infection compared with 64% of the maintenance group.
This study is the first clinical trial of therapy withdrawal in people with SLE who no longer experience symptoms on long-term MMF, according to the researchers. Their findings suggest that MMF may be safely withdrawn in many people with stable SLE, they write, but larger studies and longer follow-up are still needed.
Reference: EF Chakravarty, et al. Mycophenolate mofetil withdrawal in systemic lupus erythematosus patients. The Lancet Rheumatology DOI: 10.1016/S2665-9913(23)00320-X (2024).