New NIAID-supported science presented at the 2024 HIV Research for Prevention (HIVR4P) conference in Lima, Peru features a breadth of HIV discovery and translational findings and enriches the evidence base on HIV pre-exposure prophylaxis (PrEP) within the context of reproductive health. Select Institute-supported science highlights are summarized below. Full HIVR4P abstracts are posted on the official conference Web site.
Using PrEP Modalities Alongside Contraception and in the First Trimester of Pregnancy
The monthly dapivirine vaginal ring for HIV prevention was safe in cisgender women who used the ring during early pregnancy and then discontinued use as soon as they learned that they were pregnant. In a pre-licensure open-label study of the dapivirine vaginal ring, participants stopped using it if they became pregnant because ring use during pregnancy was beyond the scope of the study. Pregnant study participants remained enrolled after discontinuing the ring and were monitored for safety throughout their pregnancies. An analysis of data from 72 pregnancies found that there were no notable adverse effects among the participants or their infants when the ring was used in early pregnancy. These findings add to the growing evidence that the dapivirine vaginal ring is safe to use throughout pregnancy. Data presented from another study previously confirmed the safety of the ring when participants initiated use during the second trimester and continued to use it until delivery.
An analysis from the Phase 3 study of long-acting injectable cabotegravir (CAB-LA) PrEP in cisgender women found the drug did not interact with long-acting reversible contraceptive (LARC) drugs. A subset of study participants taking the LARCs etonogestrel, medroxyprogesterone acetate or norethindrone provided additional blood samples so that the study team could analyze how taking LARCs together with CAB-LA or oral PrEP with tenofovir disoproxil fumarate and emtricitabine (TDF/FTC) could affect the levels of the antiretroviral drugs and contraceptive agents in the body. There were no drug interactions between CAB-LA and any of the LARCs. Interaction between TDF/FTC and LARCs could not be determined because adherence to TDF/FTC was low in the participating cohort. CAB-LA and TDF/FTC were previously shown to be safe for use in pregnancy.
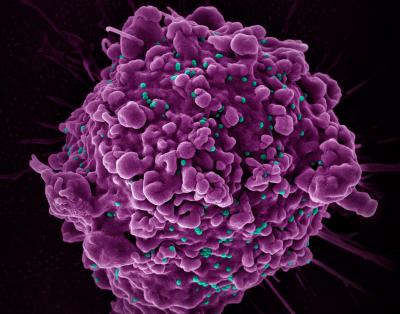
Early-Stage Findings on HIV Vaccines to Produce HIV Broadly Neutralizing Antibodies
Several studies of germline targeting—a promising HIV vaccine strategy that stimulates the immune system to generate antibodies capable of neutralizing diverse HIV strains—reported results to inform the next stages of vaccine development. Findings in people and animal models showed that several immunogens—molecules used in a vaccine to elicit a specific immune system response—began to prompt immune responses that could generate HIV broadly neutralizing antibodies (bNAbs). In one study of 53 participants without HIV, a vaccine containing a nanoparticle immunogen called 426.mod.core-C4b was safe at multiple dosing levels and appeared to generate B cells capable of producing bNAbs if stimulated further. These findings are informing the development of more advanced HIV vaccine concepts involving the 426.mod.core-C4b immunogen.
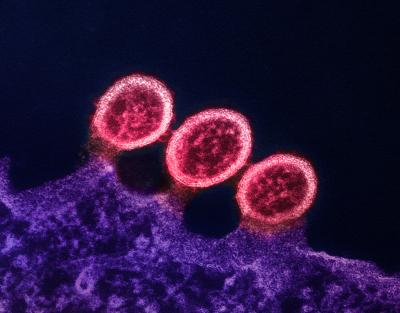
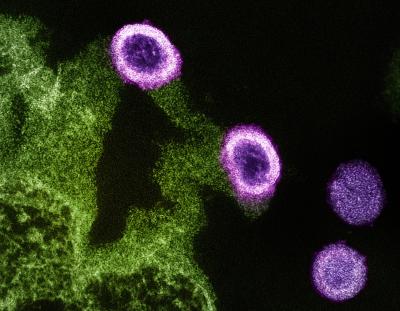
Understanding the HIV Reservoir and HIV Remission Off Antiretroviral Therapy
HIV is difficult to cure because the virus is skilled at “hiding” in the body and can reappear in the blood stream shortly after antiretroviral therapy (ART) is stopped. These hiding places, called reservoirs, are unaffected by ART. NIAID-supported scientists are exploring strategies to clear HIV and its reservoirs from the body or to reduce HIV to levels that can be suppressed by a person’s own immune system. A new small study found that monocytes—a type of white blood cell—expressing a gene called interleukin 1 beta (IL1B) are associated with smaller HIV reservoirs after a person acquires HIV. Further understanding of the influence of IL1B on HIV reservoir size could guide future novel HIV remission strategies.
Clinical trials and animal studies of HIV remission approaches reported outcomes of interventions designed to maintain HIV viral suppression or remission after ART was paused. When ART is paused in an HIV remission study it is called an analytical treatment interruption (ATI). In one study, researchers infected 16 infant monkeys with the simian version of HIV (SHIV), then placed them into three different treatment groups, each including ART with various combinations of the investigational HIV drug leronlimab and the HIV bNAbs called PGT121-LS and VRC07-523-LS. After 27 weeks of treatment, the research team conducted an ATI and observed outcomes by treatment group. Animals that received ART and both HIV bNAbs experienced rapid rebound of detectable SHIV. Two of 6 animals that received ART and leronlimab remained free of detectable virus through 20 weeks after ATI. All of the animals that received ART, leronlimab and the two HIV bNAbs remained free of detectable virus at the time of abstract submission, 15 weeks after ATI. Monitoring and assessment of monkeys’ SHIV reservoirs is ongoing, and further studies are warranted to understand the effects observed, according to the authors.
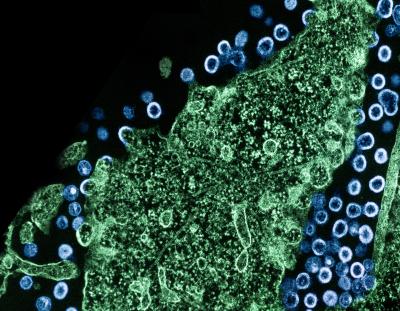
Novel PrEP Implant Technology
Available PrEP methods currently include oral pill, long-acting injectable, and controlled release vaginal ring formulations. A novel refillable controlled-release antiretroviral drug (ARV) implant was found to be safe and capable of delivering one or more ARVs. The implant, placed subdermally—just under the skin—was examined in monkeys and demonstrated that it could provide sustained release of the investigational ARVs islatravir and MK-8527 as well as the lenacapavir, which is licensed for ART and being studied for PrEP, and bictegravir and dolutegravir, both licensed for ART. Implants containing islatravir were evaluated for efficacy as PrEP and found to completely protect the animals from SHIV challenge—direct administration of the virus vaginally and rectally—through 29 months. The implant is being studied for delivery of ARVs for PrEP and ART.
HIV clinical research builds upon basic science discoveries, preclinical studies, and consultations with communities affected by HIV. Further, clinical research relies on the dedication of study participants and the people who support them. NIAID is grateful to all who contribute to advancing HIV research.
References
P Ehrenberg et al. Single-cell analyses reveal that monocyte gene expression impacts HIV-1 reservoir size in acutely treated cohorts. HIV Research for Prevention Conference. Tuesday, October 8, 2024.
W Hahn et al. Vaccination with a novel fractional escalating dose strategy improves early humoral responses with a novel germline targeting HIV vaccine (426.mod.core-C4b): preliminary results from HVTN 301. HIV Research for Prevention Conference. Wednesday, October 9, 2024.
N. Haigwood et al. Short-term combination immunotherapy with broadly neutralizing antibodies and CCR5 blockade mediates ART-free viral control in infant rhesus macaques. HIV Research for Prevention Conference. Wednesday, October 9, 2024.
M Marzinke et al. Evaluation of potential pharmacologic interactions between CAB-LA or TDF/FTC and hormonal contraceptive agents: a tertiary analysis of HPTN 084. HIV Research for Prevention Conference. Thursday, October 10, 2024.
A Mayo et al. Pregnancy and infant outcomes among individuals exposed to dapivirine ring during the first trimester of pregnancy in the MTN-025/HOPE open-label extension trial. HIV Research for Prevention Conference. Thursday, October 10, 2024.
F Pons-Faudoa et al. Drug-agnostic transcutaneously-refillable subdermal implant for ultra-long-acting delivery of antiretrovirals for HIV prevention. HIV Research for Prevention Conference. Wednesday, October 9, 2024.