The NIH Office of Research on Women’s Health (ORWH) and Office of AIDS Research (OAR), in partnership with multiple NIH institutes and centers (ICs) including NIAID, have issued a Notice of Special Interest (NOSI): Research Opportunities Centering the Health of Women Across the HIV Research Continuum to invite HIV-related research that explicitly and intersectionally center the health needs of cisgender women and girls, and gender-diverse people.
Research Objective
Data from the CDC indicate that over 250,000 women were living with HIV and more than 5,000 women newly acquired HIV in 2020 in the United States and dependent areas. Moreover, insufficient consideration of sex, gender, and their intersection, as well as limited inclusion of women and gender diverse people in health research, reduces the availability and accessibility of safe and effective HIV prevention, treatment, and cure.
The goal of this NOSI is to highlight key opportunities of research interest at the intersection of HIV and women’s health. Each participating IC has its own specific areas of research interest.
IC-Specific Research Areas of Interest
NIH strongly encourages applicants to discuss proposed submissions with the scientific contact for the proposed IC prior to submission to ensure their applications align with IC mission areas and priorities for the initiative. You can find a comprehensive list of NIH-wide research opportunities to center women’s health across the HIV research continuum in the Notice of Information: Research Opportunities Centering the Health of Women Across the HIV Research Continuum.
NIAID is interested in supporting research programs that focus on HIV and other health outcomes in women to inform and enable more targeted and effective HIV prevention and treatment. We are specifically interested in receiving hypothesis-driven research applications that can address current scientific gaps in research that will:
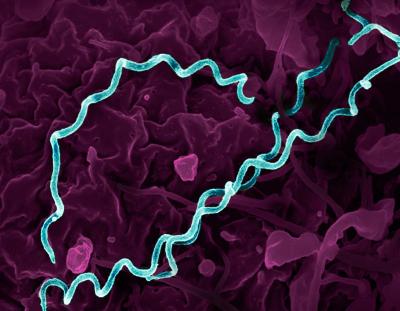
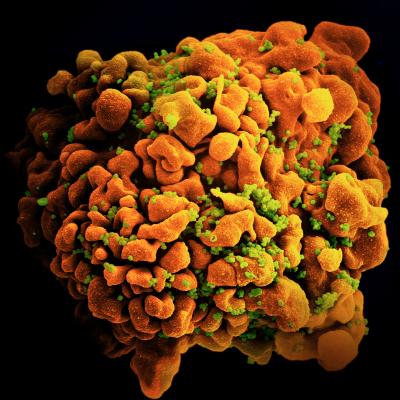
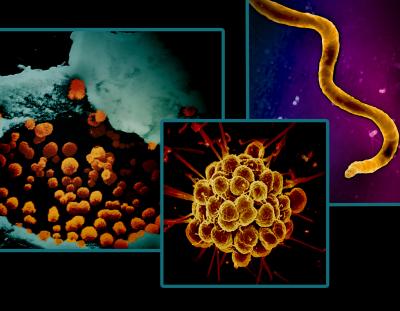
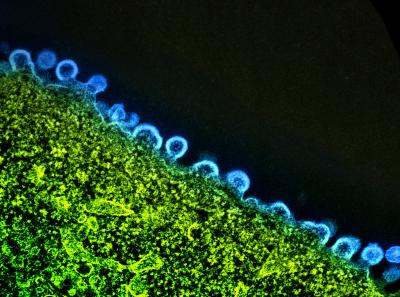
- Elucidate sex or gender-based differences in host and HIV-specific mechanisms related to transmission, susceptibility, host-pathogen interactions, innate and adaptive immune responses to infection and vaccination, including adverse events, characterization of latency, persistence, and viral reservoirs or prevention clinical outcomes.
- Accelerate development of HIV treatment and prevention modalities, including ultra-long-acting strategies for associated co-infections or coupled to contraception or hormone replacement therapy (HRT) for women across the lifespan.
- Improve understanding of the impact of menopause, pregnancy, or breast-feeding on disease pathogenesis or HIV treatment and prevention outcomes.
- Develop novel preclinical models (in-vitro, in-vivo, and in-silico) to understand sex- and/or gender-based differences that can enhance basic, translational, and clinical research focused on prevention or treatment of HIV and associated co-infections or contraception.
- Employ novel data science and analytic methods, epidemiology concepts, or enhanced dissemination and implementation of methodologies that lead to better identification of vulnerabilities, or better inform end-user data collection in or around women’s preferences or usage of HIV prevention and treatment modalities across the lifespan.
Application and Submission Information
This NOSI applies to due dates on or after June 20, 2024, and subsequent receipt dates through January 7, 2026. Refer to the NOSI linked above to find a list of relevant notices of funding opportunity (NOFOs) to apply to.
You can also submit applications to this initiative by using any reissues of these announcements through the expiration date of this notice. Note that you must select the IC and an associated NOFO to use for submission of an application in response to this NOSI.
Choose an initiative or NOFO that is appropriate to your research needs. NIAID is participating in NOFOs that span a variety of activity codes: R01, R03, R15, R21, K01, K08, K23, K24, K99/R00, F30, F31, and F32. For budget, project period, and deadline requirements, refer to the NOFO through which you decide to apply.
To be considered for funding, you must include “NOT-OD-24-119” (without quotation marks) in the Agency Routing Identifier field (box 4B) of the SF 424 R&R form. Applications without this information in box 4B will not be considered for this initiative.
Inquiries
Direct any questions to NIAID’s scientific/research contacts: Ms. Joana Roe, at jroe@niaid.nih.gov or 240-627-3213 and Dr. Kristen Porter at Kristen.porter@nih.gov or 301-761-7022.