NIAID Scientists Explore Pathways of Viral Evolution
Viruses are known to evolve quickly, in part because one generation of viral growth occurs in just minutes—an instant compared to the decades taken for a human generation to occur. This evolution happens at a vast scale, too. There are more viruses on the planet than stars in the universe. That’s trillions of trillions of viruses, all evolving at breakneck speed—and yet, researchers have found that viruses often evolve to arrive at similar genetic features. NIAID scientists recently developed new tools to understand this process in an important group of viruses called enteroviruses, which are responsible for several dangerous diseases, including polio; hand, foot, and mouth disease (HFMD); and acute flaccid myelitis (AFM). Their findings have implications for the evolution of other viral pathogens, as well.
The enterovirus that causes polio, Poliovirus, may be the most well-known. It infects the nervous system, leading to paralysis and death in severe cases. Although vaccination against polio has resulted in eradication of the virus from many parts of the world, the virus continues to emerge in some places, posing a threat to public health. HFMD is caused by different enteroviruses from a group often referred to as non-polio enteroviruses, including enterovirus A71 (EV-A71) and coxsackie virus A6 (CV-A6). HFMD is very contagious and often results in a fever, sore throat, and rash, with symptoms more commonly occurring in children than adults. Although uncommon, HFMD can result in serious complications, and so large outbreaks can raise public health concerns. In rare cases, non-polio enteroviruses such as EV-A71 and EV-D68 can also lead to AFM, a dangerous disorder of the nervous system that can result in permanent impairment. Despite the risks they pose, many enteroviruses and the diseases they cause are not well understood. It’s important for scientists to uncover how enteroviruses grow and evolve so they can develop new countermeasures against these diseases.
Patrick Dolan, Ph.D., chief of the Quantitative Virology and Evolution Unit in the Division of Intramural Research, is investigating aspects of enterovirus evolution. His research group developed a new method called SEARCHLIGHT (short for scRNA-seq–enabled acquisition of mRNA and consensus haplotypes linking individual genotypes and host transcriptomes). The method homes in on individual viruses within a rapidly evolving viral population. Using cutting-edge technology, the scientists examined the communities of viruses in single cells during viral infection. This method allows for the exploration of the concept of “viral quasi-species”—a term coined by scientists to describe how populations of viruses rapidly evolve when faced with new environmental pressures. The researchers observed how, in specific conditions, viral populations explore their “genetic neighborhood”—the possible ways they could adapt—through mutation to find more successful genetic strategies. In addition, they observed how EV-D68 and EV-A71, two distantly related members of the enterovirus family, followed common routes of evolution under similar conditions, suggesting that the routes viruses travel to explore their genetic neighborhood are shaped by common features of the viruses. Insights from this research may allow researchers to predict how new viral variants emerge and develop strategies to counter them.
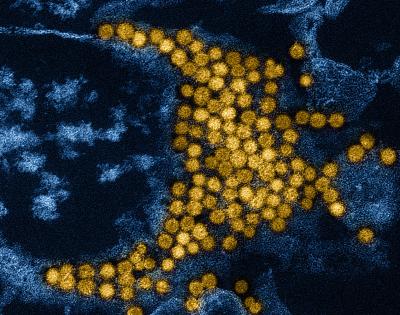
To further explore features of enterovirus evolution, Dr. Dolan’s team used an innovative method to map all the sites of the genome known to foster insertions and deletions, or InDels. InDels are major evolutionary events in which short genetic sequences can be removed or added, as opposed to single substitutions in the genetic sequence, which are minor events that generally have more modest effects on gene function. The team examined tens of thousands of mutations in EV-A71, finding that InDels were only tolerated at specific hotspots, many of which appear to be critical for adaptions in viral function and immune evasion. For instance, the researchers observed many InDels in the regions of the genome dedicated to forming the viral capsid—the outer shell of the virus that interacts with the body’s machinery to enter cells, as well as triggering an immune response. This suggests that InDels in this region provide a mechanism for the virus to adapt new ways to infect cells and trick the immune system, which are critical functions for viral propagation. Based on these findings, InDels contribute significantly to the evolution and diversification of viruses. This new map of InDel sites may provide novel avenues for investigation of viral functions and interventions against them.
These studies demonstrate the power of advanced genetic technology to explore important questions in enterovirus evolution. Because enteroviruses have genetic similarities to many other viruses, this research has further implications towards discovering mechanisms of adaptation in a range of pathogens. A deepened understanding of viral evolution will provide researchers with new ways to develop targets for vaccines, therapeutics, and other countermeasures. Additionally, this research highlights the importance of investing in basic research to into how viruses adapt and function, fostering a body of knowledge researchers can draw upon for the development of interventions against infectious diseases.
References: