This blog is adapted and cross-posted from HIV.gov.
The AIDS 2024 conference is taking place in Munich, Germany. HIV.gov is providing daily coverage. Here are four updates:
NIH
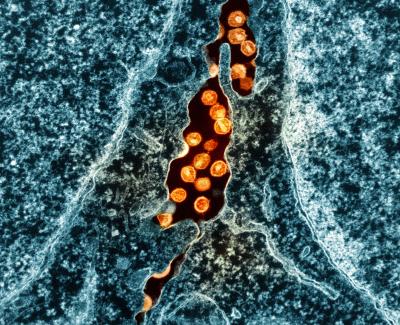
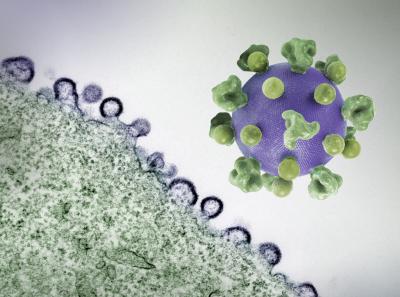
Louis Shackelford, M.P.H. of the HIV Vaccine Trials Network spoke with Carl Dieffenbach, Ph.D., director of NIAID’s Division of AIDS. They discussed the case report of the “Next Berlin patient,” a person living with HIV who is now in remission off of antiretroviral therapy following a stem cell transplant. Dr. Dieffenbach explained that this transplant was unique because both the donor and the recipient had a genetic makeup not previously seen in similar HIV cure case reports. They also discussed how this approach is only possible in unique circumstances when someone has a condition such as a cancer that requires a stem cell transplant, and discussed other approaches being explored for scalable HIV cure. Among them, he discussed the use of HIV broadly neutralizing antibodies—antibodies that bind to parts of HIV that remain relatively stable even when it mutates—in cure research. Finally, they discussed a new analysis from a large study of long-acting injectable cabotegravir (CAB-LA) for HIV pre-exposure prophylaxis (PrEP). Learn more about their conversation below:
Dismantling Inequities
Earlier in the day, Office of Infectious Disease and HIV/AIDS Policy's Kaye Hayes, M.P.A, talked with White House Office of National AIDS Policy Director Francisco Ruiz, M.S., about a panel he participated in about dismantling inequities that influence the HIV epidemic. Francisco said it is important to tailor interventions and approaches to regions and be intentional about including people with lived experience to help inform policies and programs. Learn more about their conversation below:
U=U University
HIV.gov director Miguel Gomez spoke with CDC’s Monique Carry, Ph.D., Deondre Moore and Jesse Milan, J.D., of the Presidential Advisory Council on HIV/AIDS (PACHA), about the Centers for Disease Control’s U=U University and toolkit developed in partnership with the Prevention Access Campaign and released during the pre-conference. The U=U toolkit is a community-led health message and global campaign to communicate the science behind the message of U=U, or undetectable equals untransmittable. Our colleagues also highlighted the important impact U=U is having globally and for individuals with HIV. Learn more about their conversation below:
Doxy PrEP
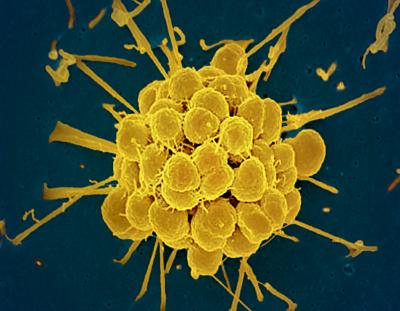
On Monday, Kaye Hayes spoke with Troy Grennan, M.D., physician lead for the Provincial HIV/STI Program, British Columbia Centre for Disease Control and Clinical Associate Professor, University of British Columbia, about research findings he shared on the potential of doxycycline as pre-exposure prophylaxis for STIs, or Doxy PrEP. While Doxy PrEP is not yet available, the work builds on previous studies. In a small pilot study of men living with HIV, researchers looked at the efficacy, tolerability, and use patterns of Doxy PrEP. They found that doxycycline was well tolerated overall, and observed 79%, 92%, and 68% reductions in syphilis, chlamydia, and gonorrhea respectively in the group who took doxycycline compared to those who took a placebo. Learn more about their conversation below:
About AIDS 2024
The International AIDS Conference is the world’s largest conference on HIV and AIDS. Held July 22-26 in Munich, Germany, AIDS 2024 brings together an estimated 15,000 scientists, policymakers, healthcare professionals, people living with HIV, and others at the intersection of science, advocacy, and human rights. The conference features more than 200 sessions, including plenaries, symposia, oral abstracts, workshops, Global Village activities, pre-conferences, and satellites. Visit the conference website for more information.
Follow, watch, and share coverage of the conference on HIV.gov’s Facebook page, Twitter/X, YouTube, and the LinkedIn page for the HHS Office of Infectious Disease and HIV/AIDS Policy.