Nearly 25 million people in the United States have asthma, including 4.7 million children and adolescents. Almost 10 percent of these individuals had one or more asthma attacks within the past 12 months. Asthma can cause coughing, wheezing, chest tightness, and shortness of breath. In severe cases, breathing becomes extremely difficult. Worsening asthma can lead to missed time at school and work, emergency room visits, and even death.
Today on World Asthma Day, NIAID reaffirms its commitment to reducing illness from this chronic lung syndrome and improving quality of life for people with asthma through research that informs the development of new asthma prevention and treatment strategies. NIAID-funded studies in children and adolescents recently uncovered new risk factors for asthma and a previously unreported cause of frequent, severe asthma attacks. In addition, two new NIAID-supported studies aim to further asthma therapeutics development by shedding light on the behavior of airway-cell genes and proteins involved in regulating asthma severity and by defining poorly understood causes of airway inflammation in underserved youth with the disorder. Learn more about these recent research highlights below.
Asthma Risk Factors
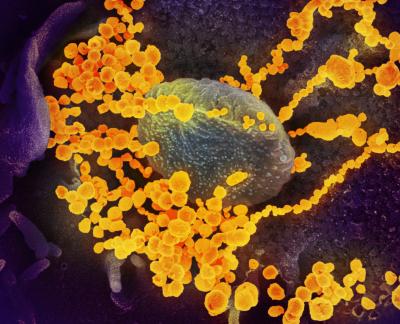
Nearly a third of infants who are hospitalized with a severe form of a common childhood lung infection called bronchiolitis develop asthma later in childhood. Predicting which infants with severe bronchiolitis are at highest risk for asthma, understanding why, and developing effective interventions remain challenges. Investigators from the NIAID-supported 35th Multicenter Airway Research Collaboration (MARC-35) recently identified genetic factors that may underlie the bronchiolitis–asthma link.
- Environmental exposures such as tobacco smoke are known to modify the function of certain genes in people, potentially resulting in long-term health effects. In one study, MARC-35 researchers examined such modifications by analyzing DNA in nasal swabs from 625 infants hospitalized with bronchiolitis. The scientists found that the genomes of some infants with severe bronchiolitis had modifications potentially caused by environmental exposures in the uterus or after birth, and these changes were associated with increased risk for asthma later in childhood. Now investigators want to identify which exposures had this detrimental effect.
- In a second study, MARC-35 researchers focused on small molecules called microRNAs, which derive from DNA and help control the genetic information that directs the building of proteins. The scientists analyzed microRNAs in nasal-swab DNA from 575 children who were hospitalized with bronchiolitis in infancy and followed until 6 years of age. The investigators identified 23 microRNAs that were turned on or off to different extents in the children who developed asthma by age 6 compared to those who did not. Now scientists want to identify what is triggering these differences and how to block them to reduce asthma risk.
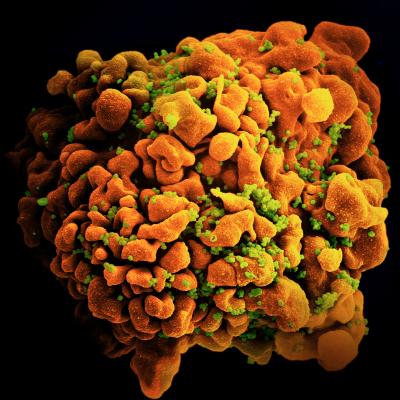
Other investigators from the NIAID-funded Urban Environment and Childhood Asthma (URECA) study linked the composition of all the microbes found in the nose—the nasal microbiota—at age 3 years to respiratory health profiles ranging from high to low risk for developing asthma by age 7 years. The scientists also found that both exposure to certain microbes in house dust during infancy and a genetic predisposition to developing allergic diseases later in childhood influence how the airway microbiota develops.
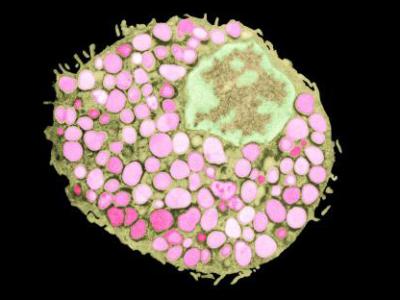
Therapeutic Insights
Scientists in NIAID’s Laboratory of Allergic Diseases recently demonstrated that a protein called RSG4 in smooth muscle cells of airway walls affects asthma severity in part by regulating airway inflammation independent of so-called G proteins. This finding builds on the lab’s 2020 discovery that blocking RSG4 in a mouse model of asthma reduced a key feature of the disease called airway hyper-responsiveness. This is a heightened sensitivity to molecules that activate smooth muscle cells in airway walls, leading to excessive airway constriction. Together the findings suggest that RSG4 in these cells could be a therapeutic target for asthma.
NIAID-supported researchers discovered recently that structural changes to nerve-cell networks in upper-airway tissues underlie asthma attacks in children who are hospitalized due to these attacks more than once a year. This contrasts with asthma attacks in children who are hospitalized less frequently, as those attacks are characterized by immune-system activity like allergic inflammation and responses to infections. The new findings, reported by the Ohio site in the NIAID-funded Childhood Asthma in Urban Settings (CAUSE) network, suggest that preventing and treating frequent severe asthma attacks in children may require an untraditional approach that targets the nervous system.
The CAUSE network also launched a new study in April 2024 to improve understanding of how airway inflammation influences asthma severity at a cellular and molecular level in children and adolescents who live in low-income urban communities. Airway inflammation in asthma may be categorized as related to a “type 2” immune response, which also plays a role in allergic diseases, or a non-type 2 immune response. The new study aims to define the cellular and molecular mechanisms associated with each type of airway inflammation in severe asthma to identify potential targets for new therapies.
NIAID thanks the hundreds of study participants and their caregivers who made these research advances possible and who help scientists continue to illuminate the complex and varied nature of asthma to reduce the burden of this disease.