Recently, the UN General Assembly held a High-Level Meeting to discuss an urgent, global public health problem: Antimicrobial resistance (AMR), which occurs when bacteria, viruses, fungi and parasites evolve to evade antibiotics and other medicines that are meant to kill them. Currently, antimicrobial resistance results in approximately 1.3 million deaths worldwide, including 35,000 in the United States each year, according to the Centers for Disease Control and Prevention. Antibiotic resistance can make infections more difficult to treat—and, unfortunately, due in part to overuse and misuse of antibiotics, antimicrobial-resistant infections are becoming more common.
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, has prioritized AMR research for many years. For instance, through the Antibacterial Resistance Leadership Group (ARLG), the Institute has supported more than 60 AMR clinical research projects, involving more than 20,000 participants at sites around the world. The results of this work, combined with 10 years of coordinated efforts from across the U.S. government, have led to significant improvements in how public health officials consider antibiotics and how physicians can tackle difficult infections. As a global, evolving problem, AMR continues to demand new research and innovations from the public health sector.
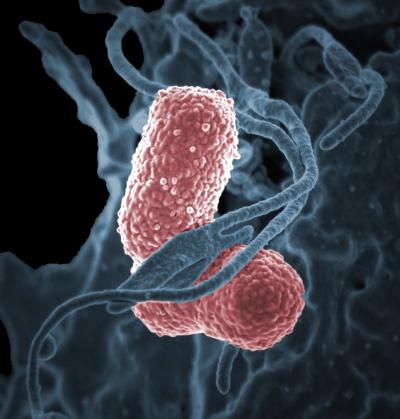
One ongoing clinical trial is examining a particularly thorny facet of treating antimicrobial resistant (AMR) infections: when dealing with antibiotic-resistant infections, healthcare providers may need to try several different treatments before they identify an effective one, and tests to verify whether treatments will work can take days to complete. This delay can slow the patient’s recovery or lead to death. For example, ineffective therapy due to treatment delay is associated with high mortality among patients with bloodstream infections caused by Gram-negative bacteria.
A new clinical trial sponsored by NIAID is currently evaluating whether the use of a rapid test of antibiotic susceptibility for bacteria growing in blood cultures improves clinical outcomes for patients with sepsis in settings that have high rates of antibiotic-resistant bacterial infections. The trial is being conducted by ARLG and will ultimately enroll roughly 900 hospitalized participants at seven locations around the world.
The Fast Antibiotic Susceptibility Testing for Gram-Negative Bacteremia Trial (FAST) will test whether use of the VITEK® REVEAL™ AST System, a direct-from-positive-blood-culture fast phenotypic susceptibility test (manufactured by Specific Diagnostics, San Jose, CA, a wholly owned subsidiary of bioMérieux, Inc., Salt Lake City, UT), can speed up the identification of effective antibiotics to treat bloodstream infections and lead to better patient outcomes. The VITEK® REVEAL™ system is already available for clinical use in the European Union (and recently received FDA 510(k) Clearance (K230675) on June 20, 2024, and can identify phenotypic susceptibility of 10 different bacteria to 23 different antibiotics. Unlike standard of care susceptibility testing, which typically takes several days to provide results, the VITEK® REVEAL™ test results are available in an average of 5.5 hours.
A recent clinical trial supported by NIAID through the ARLG showed that using a similar rapid test for antimicrobial susceptibility helped healthcare providers identify and use effective antibiotics faster than standard-of-care testing. However, that trial was unable to show whether using a rapid test led to better patient outcomes—possibly because the trial was carried out in areas with relatively low rates of antimicrobial-resistant infections. The researchers hope that data from the FAST trial will show whether the test improves outcomes in regions where many patients have antimicrobial-resistant infections.
The FAST trial has enrolled hospitalized participants with Gram-negative bacteria identified in their blood. Such bacteria include Klebsiella species and Escherichia coli. They have been randomized to one of two groups: half the participants are having their blood cultures tested with VITEK® REVEAL™ as well as standard bacterial culture and antibiotic susceptibility testing. The other participants are serving as a control group and their blood cultures will undergo standard bacterial culture and susceptibility testing. The participants’ progress is being monitored for 30 days, as clinical staff record how quickly participants recover and whether they experience any negative effects, such as worsening or relapsing while still in the hospital, requiring readmission to the hospital later for the same problem, acquiring a new infection while in the hospital, or death.
Improved testing alone will not eliminate the threat of AMR infections. For that, healthcare providers will need better therapeutics, better means of keeping the infections from spreading, and other tools. However, when patients present to the hospital with severe infections, the initial hours of waiting for test results can make all the difference. Confirming that rapid tests actually improve patient outcomes is an important step on the road to fighting back against ever-changing pathogens.
To read more about this trial, search ClinicalTrials.gov using the identifier NCT06174649.