The world of fungi includes a wide range of organisms, such as mushrooms, molds, and yeast, that are common outdoors in water, soil, and air; indoors on surfaces; and on our skin and inside our bodies. Although many fungi are helpful—or even delicious, like some mushrooms—there are many others which can cause disease. Some fungal infections are more common in people with weakened immune systems or hospitalized individuals, while other fungal infections can infect anyone, including otherwise healthy people. According to the Centers for Disease Control and Prevention (CDC), more than one billion people worldwide get a fungal infection each year. There are four main classes of antifungal drugs, and the rising rate of antimicrobial resistance is limiting and complicating existing treatment options. Currently, there are no approved vaccines to prevent fungal infections.
NIAID conducts and supports basic, translational, and clinical research to understand how fungal pathogens cause disease and how the immune system responds to infection. NIAID researchers are exploring how fungal susceptibility and infection impact the function of immune cells. The following are examples of ongoing clinical trials supported by NIAID through the investigator-initiated clinical trial funding mechanism investigating various aspects of fungal disease.
Stewardship in AMR – Examining a shorter treatment course for children
Immunocompromised patients are at risk for the development of fungal infections. Hospitalized patients can get severe, often deadly, fungal diseases like candidemia, a bloodstream infection caused by the Candida fungus. According to the CDC, candidemia is one of the most common bloodstream infections in the U.S. with an estimated 25,000 cases each year. The current treatment guidelines for invasive candidemia recommend 14 days of antifungal therapy. This guideline is based on expert opinion rather than comparative data and the optimal treatment duration remains unknown. NIAID-funded researchers Drs. William J. Steinbach and Brian T. Fisher are conducting a clinical trial (NCT05763251) to examine whether a shorter 7-day treatment strategy is just as safe and effective as current practice. This trial is only enrolling pediatric patients at the study-site hospitals with uncomplicated cases of candidemia. A shorter treatment would significantly reduce the burden of care on sick and recovering pediatric patients, allowing families to come home earlier from the hospital, and could help combat the rising rates of antimicrobial resistance. This is the first randomized control trial to explore the efficacy of a shorter course treatment for any invasive fungal disease. The trial is supported through NIAID grant funding R01 AI 170385.
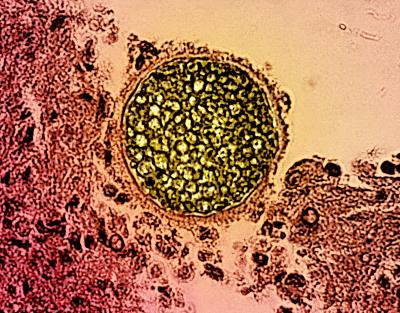
Cryptococcus neoformans contributing to HIV/AIDS-related mortality
Cryptococcus neoformans is a fungal pathogen that can cause cryptococcal meningitis. Those most at risk are immunocompromised, such as people/persons living with HIV/AIDS. Although Antiretroviral therapy (ART) has significantly reduced the incidence of HIV/AIDS in the United States, regions of the world with limited access to ART are still seeing tens of thousands of cases. According to the CDC, each year an estimated 152,000 people living with HIV experience cases of cryptococcal meningitis, of which an estimated 112,000 deaths occur, most in sub-Saharan Africa. In the weeks prior to the onset of meningitis, the cryptococcal antigen (CrAg) is detectable in the blood and is a good predictor of meningitis and death. NIAID-funded researcher Dr. Radha Rajasingham is leading a clinical trial (NCT03002012) to examine whether the treatment combination of liposomal amphotericin (AmBisome) and fluconazole for those who receive a positive CrAg antigen test effectively prevents cryptococcal meningitis and death. Dr. Rajasingham’s lab at the University of Minnesota is dedicated to improving cryptococcal meningitis treatment strategies and outcomes for people/persons living with HIV/AIDS and is supported through NIAID grant funding U01 AI 174978 and R01 AI162181.
Though these conditions can be severe, they are not the only fungal diseases of concern for NIAID. From aspergillosis to Valley Fever, NIAID is committed to researching new treatments, diagnostics, and preventative measures for a wide array of fungal diseases, especially in the face of rising antifungal resistance.