NIAID Director Dr. Jeanne Marrazzo opened the 208th meeting of NIAID’s Advisory Council by greeting Council members, as well as public representatives from professional and lay organizations who share interests and activities in common with our mission.
You can watch a recording of the Spetember 9, 2024 open session remarks at NIAID Advisory Council on NIH VideoCast.
Council Farewells and Welcomes
Dr. Marrazzo announced the end of 4-year terms for three Council members: Drs. Linda Bockenstedt, Keith Jerome, and Stephanie Taylor, and she presented them with plaques to recognize their service. She then welcomed three ad hoc members to Council: Drs. Dusan Bogunovic, Joaquin Espinosa, and Bernard Khor.
Read Biographical Sketches of NIAID Council Members to familiarize yourself with our Council members’ backgrounds.
Key Staffing News and Honors
Dr. Marrazzo noted some staffing updates within NIH.
- Dr. Caroline Hutter was named Director of the Office of Strategic Coordination.
- Dr. Geri Donenberg was named NIH Associate Director for AIDS Research and Director of the NIH Office of AIDS Research.
Then Dr. Marrazzo invited a round of applause for Dr. Hugh Auchincloss on his upcoming retirement after 18 stellar years as NIAID Principal Deputy Director, during which time he also served as Acting NIAID Director.
As part of settling into the Office of the Director, Dr. Marrazzo has been building her staff. She introduced the following new members of her leadership team:
- Dr. Lucas Buyon was named Health Science Policy Analyst and Scientific Special Assistant.
- Dr. Robert Eisinger was named Senior Advisor.
- Dr. Tara Palmore was named Senior Medical Advisor.
She noted several other staff who have joined or taken on new roles within NIAID:
- Dr. Cesar Boggiano is the new Director of the Vaccine Research Program in the Division of AIDS.
- Dr. Bruce Burnett is the new Chief of the Office of Regulatory Affairs in the Division of Allergy, Immunology, and Transplantation.
- Dr. Chelsea Boyd is the new Director of the Office of Extramural Research Policy and Operations in the Division of Extramural Activities.
Meetings and Events
Dr. Marrazzo and NIH Director Dr. Monica Bertagnolli visited Whitman-Walker’s Max Robinson Center, a community-based research site in Washington, DC, in celebration of Pride Month. The Center has been a critical NIAID resource for clinical research and prevention studies, as well as training in community-based health.
Dr. Marrazzo also highlighted what she calls “scientific diplomacy,” as the Institute hosted several meetings in town over the summer. NIAID leadership met with delegates and representatives from China, Australia, Japan, South Africa, and the World Health Organization on topics related to neglected tropical diseases, basic research, and tuberculosis, among others.
Budget News
Since fiscal year (FY) 2016, NIAID’s funding has been stable, with steady increases through FY 2024.
Looking ahead, Dr. Marrazzo noted President Biden’s FY 2025 budget request to Congress, released in March 2024, proposed an overall increase for NIH of 5.6 percent, or $2.76 billion above the FY 2024 enacted level.
In July, the House submitted an FY 2025 budget that envisioned dividing NIAID’s budget between two new ICs: a National Institute on Infectious Diseases with a budget of $3.3 billion and a National Institute on the Immune System and Arthritis with a budget of $3.3 billion. The Senate budget submitted in August proposed that NIAID receive a $130 million increase over FY 2024, which amounts to a 2 percent increase.
[Note: While NIH has not yet received an FY 2025 appropriation, a continuing resolution enacted on September 26, 2024, keeps NIH (and NIAID) funded at the FY 2024 enacted level through December 20, 2024. Also, on October 1, 2024, NIAID posted interim paylines for FY 2025 to our NIAID Paylines page.]
Dr. Marrazzo then turned to earmarks, pointing out the limited flexibility afforded by this designation to allocate funding to competing NIAID priorities. For FY 2025, both the House and the Senate proposed a $25 million increase to the tickborne disease target, above the FY 2025 enacted amount of $100 million. The Senate also proposed $80 million in funding for Antiviral Drug Discovery Centers and $10 million more to National Biocontainment Laboratories for a total of $33 million.
Legislative Activities
In June, Dr. Marrazzo participated, along with Dr. Bertagnolli, Dr. David Goff (National Heart, Lung, and Blood Institute Director), Dr. Walter Koroshetz (National Institute of Neurological Disorders and Stroke Director), and Dr. Joe Breen (NIAID Division of Allergy, Immunology, and Transplantation) in a “Lunch and Learn” on Long COVID for congressional staff.
Dr. Marrazzo briefed members of the GOP Doctors Caucus on NIH/NIAID research on H5N1 as part of a larger multiagency briefing on federal efforts related to H5N1. Representatives from the Assistant Secretary for Pandemic Responses Office, the Center for the Biomedical Advanced Research and Development Authority (BARDA), FDA, CDC, and USDA also participated.
Congressional appropriations staff visited our Rocky Mountain Laboratories (RML) in August, where Dr. Marshall Bloom, RML Director, led a site visit that included bipartisan Senate and minority House staff members who heard first-hand from investigators about RML’s broad range of research.
Scientific Updates
Emphasizing that we’re “not where we should be” with the global HIV pandemic, Dr. Marrazzo noted that epidemics are growing; incidence in several regions was higher than in sub-Saharan Africa for the first time in many years. She then discussed several recent research outcomes, including:
- Safety and efficacy of long-acting pre-exposure prophylaxis (PrEP) in studies among cisgender women and during pregnancy.
- “The next Berlin patient,” who achieved sustained HIV remission without antiretroviral therapy after a stem cell transplant.
- Multiple promising DoxyPrEP and DoxyPEP results.
- Interesting sessions on broadly neutralizing antibodies.
- Vaccine development, focusing on germline targeting.
- Continued negative impacts of stigma, discrimination, and criminalization.
Dr. Marrazzo described increases in sexually transmitted infections as “stratospheric” and discussed innovation in new strategies for notoriously difficult syphilis diagnostics, as well as effective monitoring for effectiveness of response to vaccine candidates.
Shifting to H5N1, Dr. Marrazzo noted that NIH released the H5N1 Influenza Research AgendaPDF on June 5, 2024, and shared an array of fantastic NIAID research results that have informed the H5N1 response.
Dr. Marrazzo then discussed the escalation of Mpox, which has been endemic in Africa, but has mutated and spread to the point of becoming a public health emergency. She announced the imminent release of the NIAID-Sponsored Mpox Research AgendaPDF, with a robust set of activities to include clinical studies, diagnostics, and vaccine candidates. Dr. Marrazzo acknowledged Dr. Cliff Lane and his team for their efforts in two rural areas in the Democratic Republic of the Congo.
Within the topic of COVID-19, Dr. Marrazzo zeroed in on the challenge of Long COVID and its complex pathophysiology. She pointed to the Researching COVID to Enhance Recovery—Treating Long COVID (RECOVER-TLC) initiative that will build on NHLBI’s RECOVER successes and lessons learned. RECOVER-TLC will be dedicated to running clinical trials to investigate and test Long COVID treatments.
Dr. Marrazzo shared a recently published study of malaria vaccines that not only showed impressive efficacy but specifically included women in Mali who intended to get pregnant in the next year. She noted the paradigm shift of enrolling women who might get pregnant; following them is a big step forward in reproductive health and control of infections.
Lastly, Dr. Marrazzo discussed an NIAID-funded study of a molecular basis for cognitive impairment in lupus that is potentially modifiable with anti-hypertensive medication across the blood-brain barrier, thus reducing the cascade of inflammation.
Questions and Answers
Turning to questions from Council, Dr. Marrazzo fielded a question about the regulatory timeline for the PrEP injectable and further NIAID involvement, saying that the results she mentioned are from the first Phase 1 trial, and they must complete at least two, but then should move forward quickly. She noted price may be an issue. NIAID continues to run studies through the HIV Prevention Trials Network.
Next, Dr. Marrazzo addressed a question about the range of activities she envisions for new antiviral research funding, saying the Antiviral Drug Discovery (AViDD) Centers will further the work they’re doing. The AViDD Centers are focused on RNA viruses, direct-acting antivirals, coronavirus targets, and at least one other RNA viral group.
Dr. Marrazzo responded to a question about a recent case of H5N1 infection, saying the threat level indicates that human-to-human transmission is not considered likely nor supported by evidence.
Dr. Cliff Lane also answered a question about the mortality rate of the Mpox trial mentioned above, and he clarified that the trial benefited from brisk recruitment and a large study population, which is in contrast to the usual care and recording for that community.
Updates from NIAID’s Vaccine Research Center
Dr. Ted Pierson, Director of NIAID’s Vaccine Research Center (VRC), shared a high-level overview of what VRC staff do, how they work, and where they invest their efforts; recent recruiting activities; and vignettes of some of the scientific advances that he views as particularly exciting.
Portfolio Overview
VRC’s mission is to perform basic science research to make discoveries supporting development of novel vaccines and biologics targeting infectious diseases. VRC’s founding charge was to develop HIV vaccines, though its portfolio has expanded among many viruses and related activities.
Dr. Pierson gave many examples, including work to stabilize the entry protein for respiratory syncytial virus (RSV) to make the antigen susceptible to vaccines; structure-guided vaccine design for a paramyxovirus called Nipah virus; and basic and translational research for viruses that have class II fusion proteins as well as non-envelope viruses that lack viral membranes entirely.
You can explore VRC’s work for yourself at Vaccine Research Center’s Key Disease Areas and Research Activities.
Additions to VRC Faculty and Leadership
New hires and the specialty sections VRC launched in summer 2024 include Dr. Nicole Doria-Rose, Antibody Immunity Section; Dr. Sarah Andrews, B Cell Immunobiology Section; and Dr. Tongqing Zhou, Structural Virology and Vaccinology Section. Additionally, Dr. Jason Gall is now Chief of the Vaccine Production Program and Director of VRC’s Strategic Planning and Development.
Scientific Advances
Dr. Pierson shared four vignettes of recent emphasis within the portfolio.
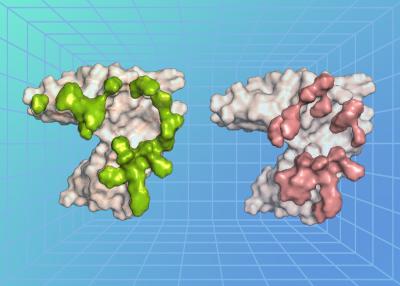
First, VRC has worked to address CAP256-VRC 26, a neutralizing HIV monoclonal antibody manufactured by VRC and tested in clinical trials in Bethesda and Africa, which is potent but lacks broad capability among various strains. The team explored building a bispecific molecule that adds new functionality to an original nanobody from a llama, which shares some binding features with human antibodies but with a smaller footprint. This model takes an antibody that is potent and adds functionality to make it broad and with better properties than the individual elements from which it’s derived. It can now neutralize 97 percent of the viruses in a panel of 208 viruses that represent the various clades of HIV. VRC will next evaluate it in clinical trials.
Second, VRC discovered a protective monoclonal antibody that binds the “dark side” of influenza neuraminidase (NA) and may inhibit infection, protect from disease, and inform potential vaccine targets. In looking back to a 2010 VRC clinical trial of an H5 DNA vaccine, B cells that made antibodies could potently neutralize contemporary influenza H5 strains. The team will test the activity of those antibodies for possible response with the avian flu circulating in cattle.
Third, while current COVID vaccines can prevent severe illness and hospitalization, they do not confer immunity to acquiring infection. VRC is exploring strategies for boosting regimens that can block infection. In primate studies, immunized chimps were boosted with either mRNA that was available to humans or mucosal delivery (intranasal or nebulizer). Intranasal antigen delivery provided profound control 4 to 5 months later; eliciting antibody response to the “right address” provided possibility of controlling virus acquisition through mucosal boosting.
Fourth, VRC is exploring antibodies that could block the malarial infection cycle by preventing parasites from getting to the liver to replicate. Preclinical studies showed that antibodies can disrupt the requisite viral proteins. One of the antibodies developed through collaborative NIAID efforts was tested (in Mali) to prevent seasonal transmission among children, and a single subcutaneous dose resulted in 77 percent protection against infection or clinical malaria. Phase 2 clinical trials are now being planned.
Subcommittee Summaries
A regular portion of each Council meeting is for scientific subcommittees to review and approve concepts for NIAID initiatives (targeted research funding opportunities). These concepts highlight NIAID’s research interests and, although not all become funding opportunities, the topics may be of interest to researchers pursuing investigator-initiated applications.
NIAID scientific staff presented our September concepts and subcommittees discussed them in the following videocast recordings:
Find text summaries of the approved concepts on these webpages: